A Professional Basketball Player not only blocks the shot but also her digestive tract, and presents with pain in the abdomen: A Case Report of Small Bowel Obstruction
A female in her 20s, a professional basketball player, presented to the Emergency Department (ED) with a severe, progressively worsening sharp pain in the abdomen for the past 7 hours. The patient graded her pain as 7 out of 10 in severity. The pain had started in the epigastric region. However, later the pain migrated to the right lower quadrant. Moreover, according to her, the pain exacerbated by movement, however, she had noticed no relieving factors. She had never experienced a similar episode of pain in her abdomen.
In the ED, she had worsening nausea and emesis. Therefore, the emergency physician started her on 4 milligrams of intravenous ondansetron and an infusion of a one litre lactated ringer bolus.
The rest of the history was unremarkable. She had no episodes/complaints of diarrhoea, constipation, fever, chills, dysuria, or vaginal discharge.
Her last meal was a self-prepared one. Moreover, she reported no recent changes to her diet, sick contacts, or recent illnesses. Her housemates and close contacts had no similar symptoms.
Pregnancy was ruled out on the basis of a recent last menstrual period and on the basis of the patient expressing a low likelihood of pregnancy. Also, the family history was negative. Additionally, she denied the use of any medications in the past or present. She denied the use of alcohol, tobacco, or recreational drugs.
On examination, her vitals were:
- Temperature: 36.8 degree Celsius
- Blood pressure: 131/65 millimetres of mercury
- Heart rate: 60 beats per minute
- Respiratory rate: 16 per minute
- Oxygen saturation: 99% on room air
General physical examination revealed that she was in discomfort, clutching her abdomen. She had a non-distended abdomen. Bowel sounds were also normal. However, the physician noticed tenderness to light and deep palpation in the right lower quadrant without guarding, rebound tenderness or tympany to percussion.
Serological investigations were normal. Moreover, the serum pregnancy test was negative. Urinalysis (UA) showed trace ketones.
A contrast-enhanced computed tomography scan of the abdomen and pelvis with IV contrast revealed distended loops of small bowel with wall thickening, enhancement, and decompressed loops of bowel distally. Moreover, it also revealed fecalization of the small bowel.
Therefore, the patient received a treatment based on the working diagnosis of an acute SBO. The treating physicians initiated NPO (nill per oral), nasogastric decompression and started her on cefazolin. A general surgery consult followed the initial management in the ED.
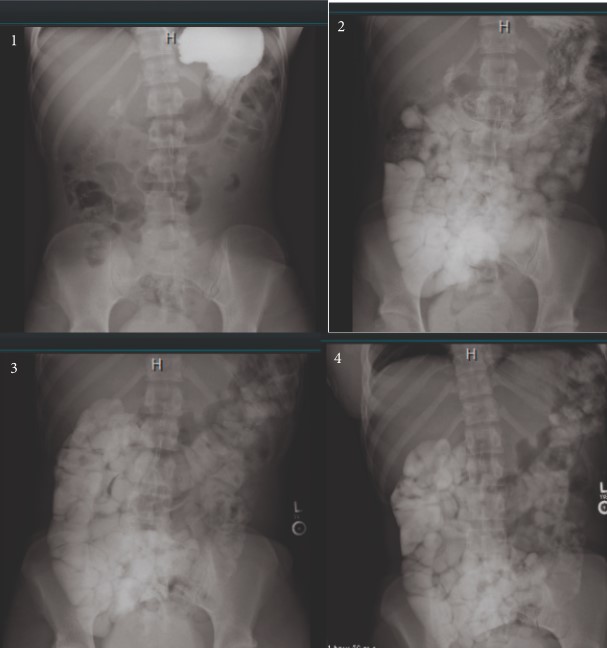
Surgeons recommended a transabdominal pelvic ultrasound (US) and a small bowel follow-through (SBFT). The US was only significant for trace free fluid in the Pouch of Douglas, and the SBFT showed resolution of the SBO at 12 hours after admission.
She started to receive a clear liquid diet. However, to evaluate the cause, the patient gastroenterology (GI) was consulted. The GI consultants progressed the patient to a soft diet and ordered a serum C-reactive protein level and erythrocyte sedimentation rate (ESR). However, both the inflammatory markers came back normal. The patient was discharged when she was pain-free and stabilised with advice to follow-up with GI as an outpatient for further workup.
Approximately, 7 days after presentation, she underwent magnetic resonance enterography which revealed no dilation, thickening, or enhancement of the bowel. GI consultants ruled out inflammatory bowel disease and other differentials. The patient’s aetiology remained idiopathic.
At 1-year follow-up, she was doing well with no recurrence.