Case Report
Selective serotonin reuptake inhibitors (SSRI) are typical psychotropic drugs. They are used to treat mental illnesses in both the community and in hospitals. A case of paroxetine-induced black hairy tongue (BHT) and necrotizing sialometaplasia (NS) in a 27-year-old woman who had been on long-term SSRIs for her mental health. Both of these lesions were treated conservatively.
Case Presentation
A 27-year-old Caucasian (British) woman appeared with a 4-month history of recurring ulcers on her soft palate. She was a light smoker and a teetotaler, with a history of von Willebrand’s disease, depression, treatment-resistant generalized anxiety disorder, social phobia, and hyperhidrosis. Despite using numerous medications such as duloxetine, sertraline, venlafaxine, trazodone, and diazepam, her mental state did not improve. She started taking paroxetine about 5 months before the ulcers developed. Histopathology found nonspecific inflammation and no signs of dysplasia.
The lesions were treated conservatively. She was given steroid mouthwashes and told to practice good oral hygiene with daily salt water gargles and chlorhexidine mouthwashes. After 19 months, she returned with a severely inflamed and ulcerated palate. As well as large debris deposits on a dark hairy tongue. Her anxiety problems did not improve with paroxetine, therefore it was discontinued.
She was put back on venlafaxine and introduced to buspirone. Interestingly, both of her oral lesions significantly improved after the discontinuation of paroxetine.
Discussion
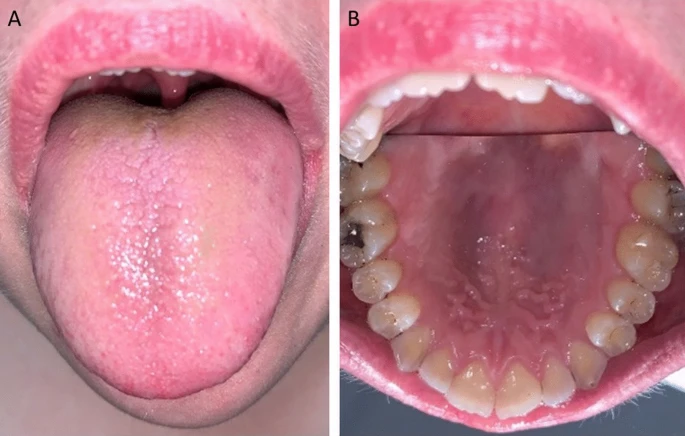
BHT, also known as lingua villosa nigra, is a reversible benign condition characterized by elongated and hypertrophied filiform lingual papillae. That stain the dorsum of the tongue. The prevalence of this illness ranges from 0.6 to 11.3%. Despite being known as a black hairy tongue, yellow, green, and brown discolorations have previously been observed. BHT is more common in male patients, with a male-to-female ratio of 3:1.
Other risk factors for BHT include old age, poor dental hygiene, xerostomia, smoking, drinking too much coffee or black tea, alcohol, cancer, and some medicines. Medications related with BHT include antimicrobials (penicillin, erythromycin, and doxycycline), anticholinergic medications, psychiatric drugs (SSRIs, thiothixene hydrochloride, and benztropine mesylate), and antipsychotics (olanzapine).
The pathogenesis of BHT is unknown; however, literature suggests that it is caused by inadequate desquamation of the dorsal surface of the tongue, which prevents normal debridement. This creates an accumulation of keratinized layers, resulting in elongation and hypertrophy of the filiform papillae. Furthermore, the entrapment of desquamating keratin and porphyrin-producing chromogenic bacteria may contribute to the discolouration.
Furthermore, SSRIs have been linked to hyperpigmentation. Serotonin has been demonstrated to stimulate melanin synthesis in melanocytes.
Conclusion
Patients with BHT are usually asymptomatic, however they may have halitosis, dysgeusia, nausea, gagging, xerostomia, and burning sensations. A clinical examination can help to make a diagnosis. These lesions can be debrided or handled conservatively (removing the causative agent and maintaining proper oral hygiene).
NS, on the other hand, is a benign, uncommon, and self-limiting reactive inflammatory illness affecting a minor salivary gland. NS is often unilateral, with the hard palate being the most prevalent location of occurrence. Lesions have also been observed on the lips, tongue, floor of the mouth, retromolar trigone, hypopharynx, and tonsillar pillars. Predisposing factors proposed in the literature include smoking, drinking, local trauma, local vasoconstriction and ischemia, medications (excessive topical nonsteroidal antiinflammatory medicines), vasculitis (granulomatosis with polyangiitis), and purging in bulimia nervosa.