Case Presentation: Ramsay Hunt Syndrome
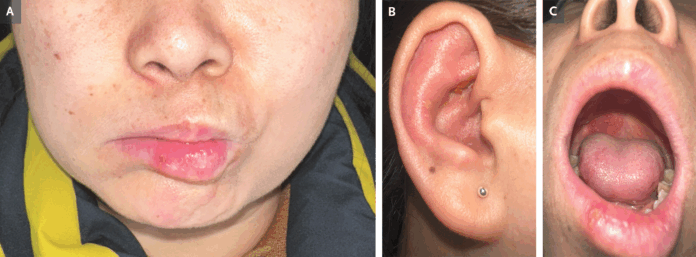
A 48-year-old woman with no prior medical history presented to the dermatology clinic with a one-day history of a rash localized to her right ear. This was preceded by two days of right-sided ear pain and an inability to move the right side of her face. On physical examination, she exhibited right-sided facial nerve palsy and erythema with several vesicles and areas of crusting on the pinna. Intraoral examination revealed vesicular lesions on the right side of the hard palate, erythema on the anterior portion of the tongue, and an ulceration on the right lower lip. Her hearing remained unaffected. Based on the clinical findings, a diagnosis of Ramsay Hunt syndrome (herpes zoster oticus) was made.
This condition results from the reactivation of the varicella–zoster virus (VZV) within the geniculate ganglion—a sensory ganglion associated with the facial nerve (cranial nerve VII) that innervates parts of the external ear and oral cavity. The syndrome typically presents with a triad of ear pain, vesicular rash in the ear or mouth, and ipsilateral facial paralysis.
The patient was started on a combination of an antiviral agent, a corticosteroid, and pregabalin for neuropathic pain. Three weeks after initiating treatment, her ear pain and mucocutaneous lesions had fully resolved. By 12 weeks, she showed significant improvement in facial nerve function, with her condition improving from a grade 5 to a grade 2 on the House–Brackmann scale (a grading system from 1 to 6, where 1 indicates normal facial function and 6 represents complete paralysis).
Pathophysiology & Epidemiology
Ramsay Hunt syndrome (herpes zoster oticus) develops when latent varicella–zoster virus (VZV)—the same pathogen responsible for chickenpox and shingles—reactivates in the geniculate ganglion, a sensory cluster within the facial nerve (CN VII) VZV can extend to the auditory (CN VIII) or other cranial nerves via shared vascular networks and neural connections . Although rare—with reported incidence around 5 per 100,000 annually, rising in those >60 years—this syndrome accounts for about 12 % of all peripheral facial paralysis cases. It affects men and women equally, and immunocompromised or stressed individuals are more at risk.
Clinical Presentation
Patients typically experience intense, deep otalgia that precedes visible signs by hours or even days pmc.ncbi.nlm.nih.gov+12emedicine.medscape.com+12termedia.pl+12. Then, the classic triad appears:
- Unilateral ear/auricular vesicular rash (pinna, external canal, or eardrum)
- Ipsilateral lower motor–neuron facial palsy, affecting muscles of expression (forehead, eye, mouth), usually reaching peak weakness by 1 week.
- Ear pain (otalgia)
These are often accompanied by mucosal vesicles—on the palate, tongue, or cheek—reflecting extension of viral spread via nervus intermedius. Additional signs may include tinnitus, vertigo, hearing loss (seen in ~50 % of cases), hyperacusis, dysarthria, headache, fever, and rarely ataxia.
In your patient, the presentation fits well: 2 days of ear pain, sudden facial weakness, vesicles on pinna, palate, tongue, and lip—but intact hearing. Her case exemplifies typical Ramsay Hunt syndrome.
Differential Diagnosis
Clinically, a diagnosis is straightforward when the triad is evident. However, absence of rash (“zoster sine herpete”) may mimic Bell’s palsy, trigeminal neuralgia, or vestibular schwannoma. Laboratory confirmation via VZV PCR or viral culture from vesicle fluid, saliva, or tears is possible but often unnecessary in clear-cut cases. Basic labs (CBC, ESR, electrolytes) help rule out other inflammatory or infectious etiologies .
Neuro‑otologic exams (audiometry, vestibular tests) and MRI may be warranted if symptoms persist or involve additional cranial nerves.
Ramsay Hunt syndrome generally has a less favorable prognosis than Bell’s palsy Prognostic factors associated with poorer outcomes include:
- Age over 50
- Complete facial paralysis at onset
- Presence of vertigo or additional cranial nerve involvement
- Unexcitable facial nerve on neurophysiological testing.
Recovery rates vary: only 10–22 % of those with severe palsy achieve full resolution, whereas up to 66 % with incomplete paralysis may fully recover. Early combined antiviral and steroid therapy improves facial nerve recovery compared to steroids alone.
Your patient’s outcome mirrors typical recovery: by 3 weeks, rash and ear pain resolved; by 12 weeks, House–Brackmann grade improved from 5 (severe) to 2 (near-normal) function.
Complications & Long-Term Follow‑Up
Potential long-term issues include:
- Postherpetic neuralgia, reported in some patients
- Persistent facial weakness, synkinesis (abnormal facial movements)
- Expanded neuropathy, involving CN V, VIII–XII or even cervical roots
- Corneal damage, taste disturbances, hearing loss, tinnitus, vertigo
- Rarely: meningitis, brainstem encephalitis
Therefore, periodic follow-up is essential to address evolving symptoms, rehabilitation, and eye protection. Patients with incomplete recovery by 3 months may benefit from facial physiotherapy or further specialist intervention.
Ramsay Hunt syndrome represents a reactivation of VZV in the facial nerve’s geniculate ganglion, presenting with pain, vesicles on the ear or oral mucosa, and ipsilateral facial paralysis—often with auditory or vestibular symptoms. Early diagnosis and treatment, typically with antivirals and corticosteroids initiated within 72 hours, significantly improve nerve recovery and reduce complications. While many achieve substantial improvement, some remain left with residual deficits or chronic neuropathic pain. Vaccination and prompt therapy are key preventive strategies.
References