Researchers at the Netherlands Cancer Institute accidentally discovered a new organ while scanning prostate cancer patients with a recently introduced imaging scan.
It seems that despite centuries and centuries of cutting up humans, doctors have missed out on an organ situated deep inside the human head.
Dr. Wouter Vogel, along with his team, was examining prostate cancer patients with a new imaging modality when he stumbled upon the new organ.
PSMA PET/CT, or positron emission tomography/computed tomography with prostate-specific membrane antigen ligands, is a newly introduced imaging study. Prior to the scan patients are injected with radioactive glucose. This causes tumors to light up during the scan. Thus, helping to monitor the spread of cancer in patients.
However, while conducting the scans researchers discovered an unexpected area lighting up among all the patients. Two bright spots appeared at the back of the nasopharynx in all scans.
The macroscopic structure showed a ligand uptake similar to that of major salivary glands. After ruling out an anomaly, the researchers concluded it as a set of salivary glands.
Source: Valstar et al., Radiotherapy and Oncology, 2020
Tubarial Glands – The New Mysterious Organ
A human cadaver study confirmed the histological and morphological features of the organ. According to the study published in the journal Radiotherapy and Oncology, both the cadavers possessed the bilateral structure. Furthermore, it confirmed the presence of mucous glands within the structure, with multiple draining ducts.
The two new areas that lit up turned out to have other characteristics of salivary glands as well. We call them tubarial glands, referring to their anatomical location [above the torus tubarius].
Dr. Matthijs Valstar, University of Amsterdam
According to medical literature humans only possess three sets of large salivary glands along with thousands of microscopic salivary glands. Their secretion, saliva, plays a role in chewing, tasting, swallowing, and digestion.
Radiotherapy during the treatment of head and neck cancers or brain metastasis can damage these salivary glands. Thus, resulting in painful swallowing, speech problems, and an increased risk of caries.
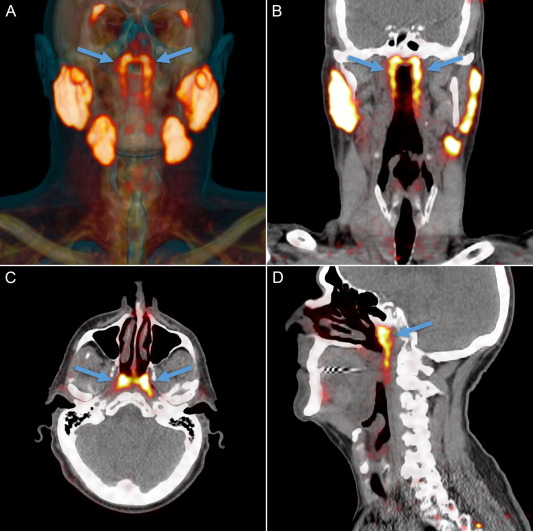
Source: Valstar et al., Radiotherapy and Oncology, 2020
The team believes avoiding radiation in the area of the Tubarial glands can protect a patient from experiencing more complications of treatment. To support their hypothesis, the team analyzed a total of 723 patients who had received radiotherapy in the designated area. The patients suffered more complications following therapy with radiation.
Our next step is to find out how we can best spare these new glands and in which patients. If we can do this, patients may experience less side effects which will benefit their overall quality of life after treatment.
Dr. Wouter Vogel, Netherlands Cancer Institute
How did we miss it?
The newly discovered organ is located under the base of the skull, an area only accessible via nasal endoscopy. Additionally, conventional methods of imaging such as CT and MRI scans are unable to interpret the submucosal structure as a salivary gland.
In conclusion, these previously overlooked bilateral salivary glands can help improve the quality of life of cancer patients. However, the authors of the study believe further research is required to validate their findings.
Reference:
M.H. Valstar, B.S. de Bakker, Roel J.H.M. Steenbakkers et al., The tubarial salivary glands: A potential new organ at risk for radiotherapy, Radiotherapy and Oncology, https://doi.org/10.1016/j.radonc.2020.09.034