Neuromyelitis Optica, SLE and hypercapnic respiratory failure
This article highlights the case of hypercapnic respiratory failure caused by systemic lupus erythematosus and neuromyelitis optica. Neuromyelitis Optica (NMO) is a rare neurological disorder that was first described by Eugene Devic in 1894. The disease was previously referred to as Devic’s disease. Earlier, the disease was also thought to be a subtype of multiple sclerosis (MS). However, with the discovery of anti-aquaporin 4 antibodies (AQP-4 Ab), it is now known as a separate disease. The disease is often misdiagnosed because of its different presentations that include blindness, weakness and spasm in the extremities. In some cases, vomiting, and bowel and bladder dysfunction may be present.
NMO is more commonly diagnosed in women and has a prevalence of 0.5 to 4.4 per 100,000 people. The onset of the disease is typically between 35 and 42 years of age. NMO is also found to be linked with other auto-immune diseases and can occur as a primary autoimmune disorder. It can occur in patients with existing systemic lupus erythematosus (SLE). In autoimmune syndromes, the destruction of tissues is immune-mediated. The same is the case with NMO. However, in the case of hypercapnia respiratory failure, the pathophysiological result is demyelination and axonal damage. The neural tissue that is damaged is primarily the optic nerve and spine.
Case study
This case study highlights the importance of correctly diagnosing NMO, especially in patients with existing autoimmune diseases. In this case SLE and NMO overlap. A delay in the appropriate management of the disease can cause short- and long-term adverse patient outcomes.
A 54-year-old black woman presented to the emergency department with complaints of chest pain, paresthesia in her bilateral feet, diplopia, generalised weakness and dysphagia. The patient’s medical history was significant for asthma and gallstones. On examination, her blood pressure was 135/80, heart rate 69 and body temperature 36.8°C with an oxygen saturation (SpO2) of 99% while the patient was breathing in ambient room air.
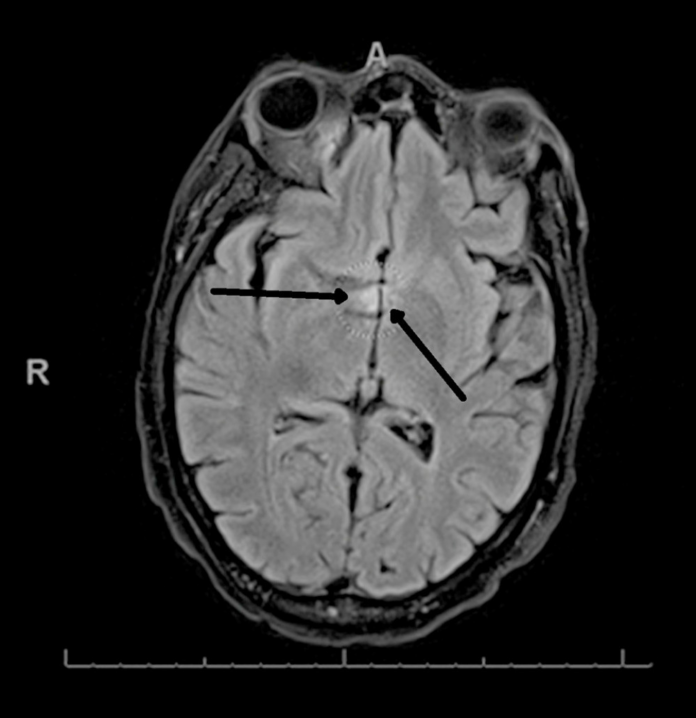
Doctors performed a computed tomography angiography on the patient. Findings of which showed an acute pulmonary embolism. The initial examination, however, did not show any focal neurologic deficits. Doctors further performed a computed tomography angiography which showed an acute pulmonary embolism. In addition, the patient’s ejection fraction was 35% to 59%. MRI of the brain showed an area of hyperintensity in the cervical medullary junction.
The patient was further referred for a full infectious and autoimmune workup from serum and cerebrospinal fluid studies. Serologic testing was positive for speckled anti-nuclear antibody of 1:160 and SSA, dsDNA antibodies, smith-RNP, chromatin and SSA. The findings are consistent with the diagnosis of systemic lupus erythematosus. Doctors started the patient on methylprednisolone 1000 mg daily for suspicion of SLE myelitis. However, the patient’s symptoms showed little to no improvement during treatment. The patient also began to show laboured breathing and worsened symptoms of nystagmus (involuntary side to side, up and down or circular movement of the eye). The blood analysis was also positive for AQP4-Ab which are a hallmark in NMO.
Treatment and prognosis
Doctors treated the patient with 5 days of plasma exchange after which she was discharged to inpatient rehab while on prednisone 40 mg daily. However, 25 days into the rehabilitation, she was unresponsive and developed acute hypercapnic respiratory failure. The patient did not exhibit any symptoms of acute asthma exacerbation before the acute respiratory failure.
On examination, her PCO2 was 102 on arterial blood gas. She was encephalopathic and had to be intubated and transferred to an intensive care unit for ventilatory support. Doctors ruled out the acute decline being related to an underlying asthma exacerbation. She was started on rituximab infusion and remained intubated for 8 days. The patient was extubated and discharged back to inpatient rehabilitation. There was barely any clinical improvement in her presenting neurological symptoms after the administration of steroids, 2 doses of rituximab, plasma exchange and intravenous immune globulin. Though her respiratory status showed improvement. Since there was a lack of improvement and worsening of findings on the second MRI of the brain, the patient was started on cyclophosphamide and oral prednisone. As recommended by a neuroimmunology specialist. The patient was gradually tapered of the meds and discharged home.
Source: American Journal of Case Reports



