A female patient developed muscle weakness and fever after she got COVID-19 pneumonia
A 63-year-old female patient with a confirmed diagnosis of COVID-19 Pneumonia was admitted to the intensive care unit (ICU) for 50 days. The patient required prolonged mechanical ventilation. During her admission, she had renal failure warranting dialysis. Moreover, the patient developed a fever and distal muscle weakness without cranial nerve involvement (quadriparesis). She also had global areflexia with sphincter control.
The patient’s medical history was significant for hypertension and hypothyroidism. Besides, the rest of the history was unremarkable.
On admission, she was conscious, alert, oriented, afebrile (36.5 ℃), with a blood pressure of 130/75 mmHg, heart rate of 88/min, respiratory rate of 18/min, and oxygen saturation of 92%. Also. there were no signs of respiratory distress
Neurological examination revealed normal cranial nerve function without alteration. However, motor examination revealed flaccid quadriparesis. Lower extremities showed more deficit than the upper limbs with 0/5 muscle strength in the former and 2/5 in the latter. Additionally, the patient had distal and generalized areflexia, with a bladder catheter and complete rectal sphincter control.
Sensory examination showed a patchy hypoesthesia in the lower extremities and perineal region. Moreover, examination revealed pressure ulcers on the sacrum, malleolar region of the right lower extremity, and the right scapula. Also, examination revealed necrotic lesions in the right hallux’s pulp and dorsum. There were traces of scarring without signs of infection.
Serological investigations showed:
- Hemoglobin: 11.2 g/dL
- Hematocrit: 35%
- Total leukocyte count: 16,400/mm3 (neutrophils: 60.4%, lymphocytes: 32.6%)
- Creatinine: 0.37 mg/dL
- BUN: 16.4 mg/dL
- Alkaline phosphatase: 93 U/L
- Potassium: 3.88 mE/L
- Sodium: 142 mE/L
- Total protein: 7.04 g/dL
- Alanine aminotransferase (ALT): 29.4 U/L
- Aspartate aminotransferase (AST): 30.5 U/L
- Procalcitonin: 0.08 ng/dL
- Creatine kinase (CK): 41 umol/L
- Partial thromboplastin time: 33.8 sgs (control 28.2 sgs),
- Thrombin time: 13 sgs (control 11.9 sgs)
- Urine culture > 100,000 Escherichia Coli colonies
- Blood cultures: Negative
The patient’s repeat PCR for the detection COVID-19 was negative by now. However, ANTI-SARS-CoV-2 IgG Antibodies were positive. But ANTI-SARS-CoV-2 IgM Antibodies were negative.
Imaging:
Plain radiograph of the chest showed hyperventilated lungs without radiological signs of an acute active inflammatory process. Moreover, a computed tomography scan of the brain and cervical spine showed subcortical, frontal and parietal granulomatous calcifications. However, there were no inflammatory signs.
Magnetic resonance imaging of the brain showed a small, subcortical, isolated, hyperintense focus in the white matter.
Plain radiograph of the left elbow was performed as the patient developed pain and functional limitation in the left elbow. The Xray showed an old fracture in consolidation with an enhancement of the distal humeral cortex. Also, the MRI of the elbow showed hyperintensity in the medial and lateral epicondyle. Thus, the orthopaedics immobilized the joint and prescribed analgesics.
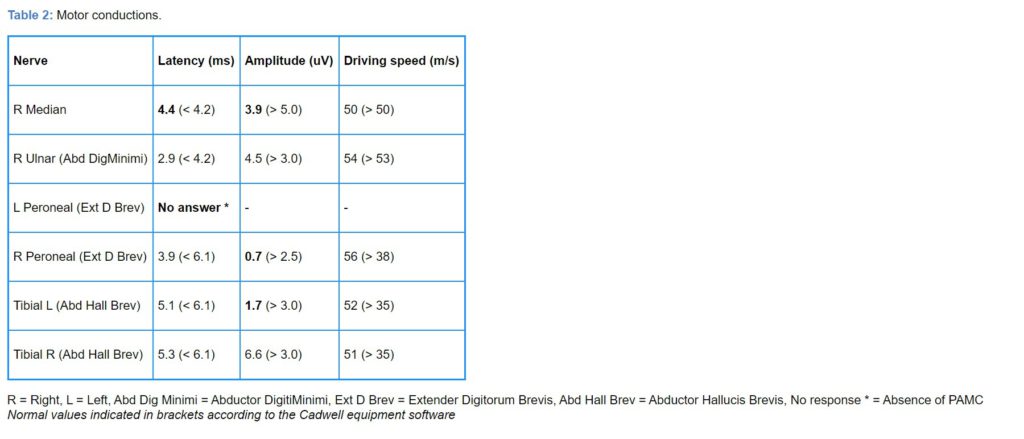
To evaluate the muscle weakness, on the 8th day of hospitalization, the electrophysiological study was performed which showed the following results:
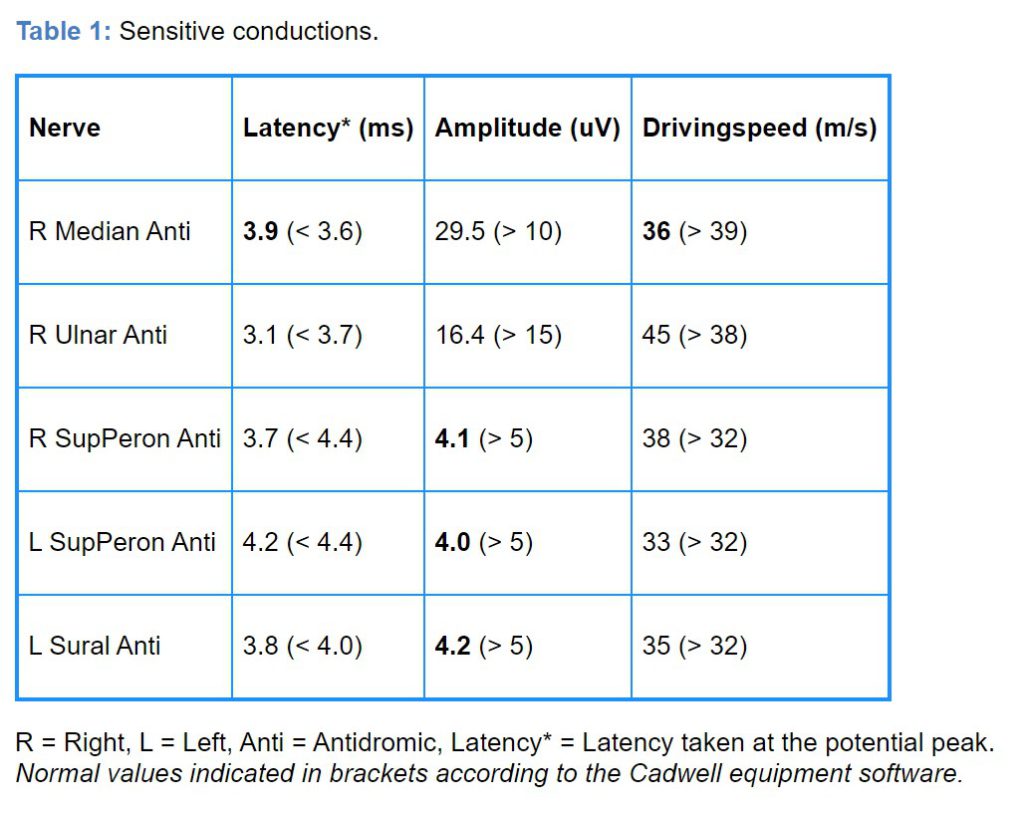
An electromyogram revealed increased insertion activity with signs of membrane instability (fibrillations 1+ and acute positive waves 2+) in bilateral Tibialis Anterior, left gastrocnemius, extensor Hallucis Longus, with motor units. The recruitment pattern decreased in these muscles.
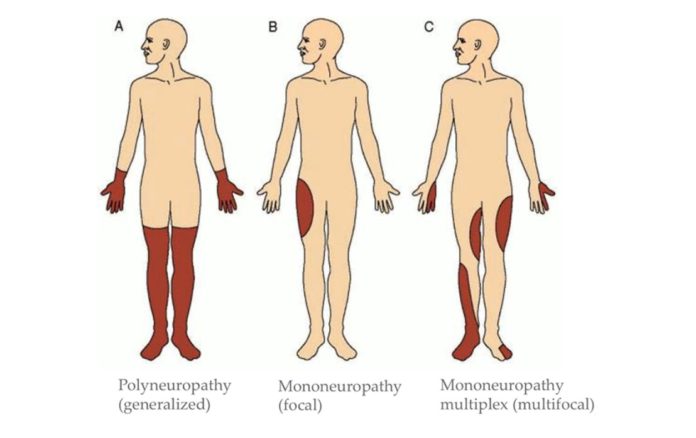
The patient received a diagnosis of Mononeuritis Multiplex, possibly secondary to renal failure and a potential vasculitis process.
Reference:
Estévez-Rivera E, Benavides-Hinestroza J, Rubiano H, García-Perdomo HA (2020) Mononeuritis Multiplex Associated with Sars-Cov2-Covid-19 Infection: Case Report. Int J Neurol Neurother 7:102. doi.org/10.23937/2378-3001/1410102