Case Report
Mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (ACC), and acinic cell carcinoma (AciCC) are among the most commonly diagnosed salivary gland cancers. Histologically, MEC is defined by a combination of three different cell types: mucus-secreting, epidermoid, and intermediate cells. These cell types work together to give MEC its particular pathophysiology. MEC rarely appears in cutaneous areas, however it frequently starts in the salivary glands.
Particularly rare, primary cutaneous MEC is believed to result from ectopic salivary gland tissue that is lodged in the skin.
In this case study, the significance of early detection and prompt identification of this uncommon cutaneous cancer is highlighted. It describes a rare presentation of primary MEC on the scalp that lasted for over ten years before exhibiting significant clinical alterations.
Case Presentation
A 49-year-old African American woman who has a history of scalp masses and came to our outpatient neurosurgery clinic. The mass, which started out as a tiny lump only a little bit smaller than a tennis ball. It has been there for more than ten years. However, it was removed at a primary healthcare institution in the suburbs about five months ago. The lesion was nontender and nonprogressive; sadly, the tissue was not sent for histological analysis. During the five months after excision. The lesion returned, became larger over time, and became ulcerated, prone to bleeding easily when touched.
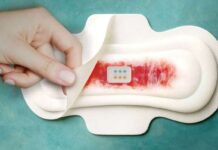
Upon clinical assessment, the patient showed no symptoms of pallor or jaundice and was alert and completely cognizant. Her vital signs were within normal limits, and there was no peripheral lymphadenopathy. Two separate masses were found on the right side of the head upon local inspection. The larger tumor, which measured around 9 × 7 cm and was fungating, was sensitive, prone to bleeding, and somewhat movable. The second lesion was non-fungating and was about 3 × 3 cm (Fig. 1A).
Investigations:
Her biochemical lab results showed normochromic normocytic red blood cells with a hemoglobin level of 13.8 g/dL, and a normal platelet count. A normal chest X-ray and unremarkable abdomen and pelvic ultrasound results were part of the imaging examinations. A multilobulated hyperdense ulcerative scalp lesion measuring 9 × 7.8 × 6 cm was discovered on the right frontal region of the scalp by a head and neck computed tomography (CT) scan.
Interestingly, neither intracranial expansion of the tumor nor degradation of the skull bone were seen. At levels I and II, there were enlarged cervical lymph nodes on both sides. Furthermore, a pathological compression fracture of the T10 vertebral body without canal stenosis was revealed by magnetic resonance imaging (MRI) of the spine, which increased the likelihood of vertebral metastases. The American Joint Committee on Cancer (AJCC) determined that she had clinical advanced stage illness (IVc), with both distant and local-regional metastases.
A lesion biopsy confirmed the diagnosis of mucoepidermoid cancer. The patient was then given advice and gave his or her consent for surgical treatment. Under general anesthesia, the lesion was removed using a wide local excision technique to guarantee total removal (Fig. 1B, C). Sterile medicated paraffin gauze was used to patch the defect. Histopathological analysis of the removed tissue confirmed the initial biopsy result of invasive mucoepidermoid carcinoma.
Following surgery, the patient was sent to the Ocean Road Cancer Institute for more testing, including a PET scan and possible radiation treatment. The patient had no symptoms related to the central nervous system and no clinical indications of recurrence at the 8-month follow-up following excision. Plastic surgeons are monitoring the scalp wound, and the pathological vertebral fracture stayed stable without the need for surgery. This favorable result emphasizes how well the initial surgical procedure and subsequent care went.
Conclusion:
Mucoepidermoid carcinoma (MEC) is a well-known tumor that makes up around 30% of all malignant tumors of the salivary glands. On the other hand, cutaneous involvement occurs occasionally.
It is unknown what causes primary cutaneous MEC. Given their parallels in the genesis of the embryonic germ layer, histological features, and functions, it has been proposed that salivary glands are descended from sweat glands. Numerous authors have also argued that the fetal precursors of sweat and salivary glands are similar to the cutaneous mucin-secreting glands found in amphibians. Therefore, it is hypothesized that an ectopic salivary gland generated from a sweat gland may have given rise to primary cutaneous MEC.
There are very few cases of primary cutaneous mucoepidermoid carcinoma (MEC) reported in the literature, making it an extremely uncommon condition. Histologically, this tumor is distinct due to its mixture of mucus-secreting and epidermoid cells. Since MEC typically starts in the parotid glands, its cutaneous manifestation is uncommon.