A team from Nottingham Trent University and Nottingham University Hospitals NHS Trust has created a new biosensor. That can reliably monitor the status of a chronic wound.
Wounds are a growing health care issue affecting thousands of people in all health and social care settings. It results in escalating costs for an already overburdened health system.
One of the most pressing demands in wound management is the development of methods that enable clinicians to detect early progression or deterioration of wounds.
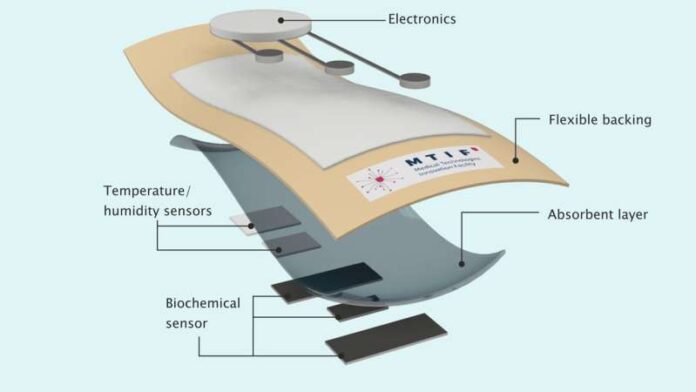
The goal, according to the team of engineers and clinical academics at NTU and NUH, is to embed the technology inside dressings. So that they do not need to be removed. And replaced on a regular basis to check how a wound is healing.
They believe that the technology—a textile-based printed protein sensor—will eventually help to lower the chance of patients becoming very ill, save amputations, and save time and money.
Patients cannot now determine the status of a wound, and health professionals must remove the dressing to inspect it visually.
This can take time since patients need an appointment. And removing the bandage too soon risks prolonging the healing process, exacerbating scarring, or introducing an infection. The dressing also needs to be changed every time the wound is examined, which takes more time.
Chronic wounds are those caused by major damage or trauma, ulcers, pressure sores, and diseases like diabetes.
The new fabric-printed sensor continuously analyzes specific protein concentrations in a wound. Patients can use an app to read the data by holding a smartphone near the dressing. It enables them to book appointments with a clinician if needed.
The miniature sensor, which is lightweight and flexible, could tell if the dressing needs any change or removal completely, or if the wound was infected.