Case Presentation
A 37-year-old Indonesian woman was admitted to the emergency department (ED) at 36 weeks gestation in her second pregnancy. She was complaining of shortness of breath that had worsened the day before. For the past two months, she had a fever and hemoptysis. Moreover, she complained of painful swallowing and hoarseness (signs of laryngeal oedema). She also had deteriorating gastroesophageal reflux disease (GERD) which hadn’t been treated. Moreover, she had a history of thyroidectomy 2 years prior, due to thyroid cancer.
She had a respiratory rate of 26-30 breaths per minute and a SpO2 of 98% with nasal oxygen supplementation. Her pulse rate was 110-120 beats per minute, and her blood pressure was 172/92 mmHg when she arrived. Doctors treated her with ceftizoxime 1g and furosemide 20 mg. They admitted her to the intensive care unit (ICU).
Due to the patient’s preeclamptic status and stridor, doctors suspected laryngeal oedema in the ICU. This was initially treated with an empirical methylprednisolone injection of 125 mg and nebulized epinephrine. To treat GERD, doctors kept her on pantoprazole 40 mg injection. Doctors performed intubation due to her deteriorating condition with worsened tachypnea, decreased oxygen saturation, and inability to talk.
Investigations
The prenatal ultrasound revealed a single living intrauterine fetus with a normal fetal heart rate. There was no cervical dilation at 36 weeks of gestation.
Laboratory testing revealed 17,000/L leukocytosis and proteinuria. Albumin, electrolytes, and coagulation profile were all within normal limits. In the emergency room, a preliminary diagnosis of pneumonia or heart failure was made. However, chest X-ray revealed no evidence of infiltrates or pulmonary oedema, and echocardiography revealed normal left and right heart function.
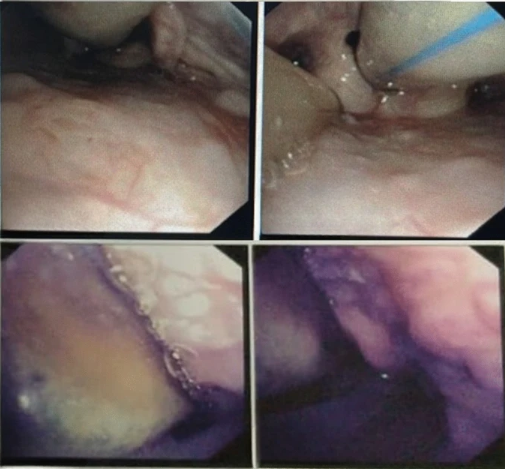
Her doctors performed fiberoptic bronchoscopy the following day which showed unevenly granular vocal cords with numerous white plaques and a bloated red look from laryngeal oedema. They stopped Methylprednisolone and commenced fluconazole at 400mg as the findings suggested fungal infection.
Prognosis
The patient was given the choice of having a tracheostomy because the use of a small-sized ETT was anticipated to be temporary. Nevertheless, since a cesarean section was safer for the fetus and laryngeal oedema typically gets better after delivery. Hence it was decided the delivery will be after 36 weeks (once the lung had matured).
Even though the patient was still on ETT, she was extremely cooperative, hence spinal anaesthesia was administered rather than general anaesthesia. The doctors also administered hyperbaric bupivacaine 10 mg with fentanyl 25 g via the L4/L5 interspace. There were no intraoperative complications. She was readmitted to the ICU after surgery with no noteworthy complaints. Her clinical and vital signs were stable 48 hours after delivery
Moreover, the patient was extubated after the positive cuff-leak test. It is a simple method for predicting post-extubation stridor. The test is carried out by deflating the cuff and measuring the expelled tidal volume (VT) a few breaths later.
She was then transported to the postpartum ward. During the bronchoscopy, a sample of laryngeal lavage fluid was obtained for culture, and the results were returned a week later with Enterobacter aerogenes.
After two days of in-patient treatment, she was discharged. She returned to the hospital for a post-discharge check-up two weeks later, and her condition had improved. The baby was also doing well.
Conclusion
This case highlights an important condition which can be life-threatening called laryngeal oedema during pregnancy. It can be brought on by upper respiratory tract infections. Securing the patient’s airway, the safety of the fetus, and the patient’s long-term health implications should all be carefully taken into account while choosing between conservative and vigorous urgent airway management.
Discussion: Laryngeal Oedema
This case report discusses how a 36-week pregnant woman was diagnosed with preeclampsia after developing high blood pressure and proteinuria. Doctors initially attributed dyspnea with fever and cough to heart failure or pneumonia, but the results of a chest X-ray and an echocardiogram were normal. They found laryngeal oedema to be the source of dyspnea with stridor in the intensive care unit, which was confirmed during intubation.
During pregnancy, the airway system is affected by physiological changes in the body. The increase in permeability and alterations in the microvasculature of the lamina propria just below the laryngeal mucosa is caused by the rise in estrogen and progesterone. Laryngeal mucosal oedema normally resolves after delivery, but it can occasionally remain. Certain conditions like pre-eclampsia, cause generalized edema in the body due to fluid retention. This can increase the risk of laryngeal oedema. However, preeclampsia-induced laryngeal oedema is uncommon. Laryngitis and a history of thyroidectomy are also risk factors for developing laryngeal oedema.
The patient had a history of thyroidectomy after which she frequently complained about hoarseness and the common cold. After this surgery, there is a danger of recurrent laryngeal nerve injury, which could result in vocal cord paralysis and thus can increase the risk of infection in the upper respiratory tract. Viruses are the most common cause and are indistinguishable from bacterial infections. The fungal infections are also common yet underdiagnosed and manifest as whitish speckling of the supraglottis or glottis, diffuse laryngeal erythema, and oedema.
The treatment of laryngeal oedema differs according to its severity and origin. Patients with a clogged airway should be treated right away. Inhalation of methylprednisolone and epinephrine has been used to treat post-extubation laryngeal oedema. The role of antibiotics is still debatable and only indicated in the case of infection.
GERD with Laryngeal Oedema
In this case, laryngeal oedema could have been caused by multiple factors. The patient had a history of GERD for a long time and it got worse in the previous two months.GERD affects 30-50% of pregnant women and worsens during the third trimester due to increased abdominal pressure, delayed stomach emptying, and decreased lower oesophagal sphincter tone caused by progesterone.
This type of gastroduodenal reflux may cause direct injury to the laryngeal mucosa. Treatment for this illness during pregnancy includes lifestyle and nutritional changes; however, more severe symptoms may necessitate medication therapy. Such as Lansoprazole, a proton pump inhibitor (PPI), which was prescribed to this patient. This medication class is now the most efficient inhibitor of stomach acid secretion.
Many cases of laryngeal oedema during pregnancy require a tracheostomy and pregnancy termination under general anaesthesia. However, because the patient could breathe comfortably with the ETT in place, doctors decided to postpone the tracheostomy. As a result, they performed the cesarean section after establishing the fetus’s lung maturation, taking into account the risk of tracheostomy and the safety of the fetus. This is important to ensure as failure to conduct a tracheostomy may result in airway blockage and reduced oxygenation of both the mother and the fetus.
Thereafter, with the administration of antibiotics, anti-inflammatory medications, and a proton pump inhibitor, the patient’s condition improved.