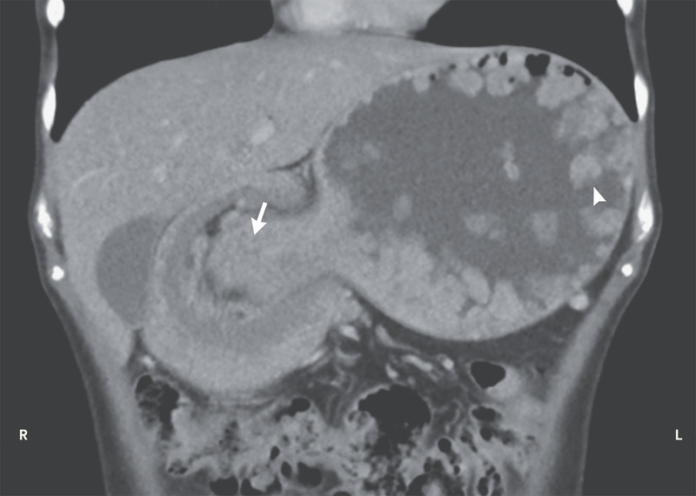
Intussusception in 26-year-old woman with a known history of Peutz-Jeghers syndrome
Peutz-Jeghers syndrome is an inherited autosomal inherited condition that presents with hyperpigmented mucocutaneous macules and hamartomatous polyps in the digestive tract. It further increases the risk of gastrointestinal and non-gastrointestinal cancers. This article describes the case of a 26-year-old woman with a known history of Peutz-Jeghers syndrome. The patient presented to the emergency department with a 1-week history of nonbilious vomiting and abdominal pain.
On examination, the patient’s heart rate was 110 beats per minute and blood pressure 120/90 mm Hg. Palpation of the abdomen was consistent with a tender mass in the upper abdomen. Doctors further advised a computed tomography of the abdomen, findings of which showed multiple gastric polyps and gastrogastric intussusception which extended into the duodenum. Although uncommon, gastrogastric intussusception is a serious complication of Peutz-Jeghers syndrome.
The patient was referred for an emergency laparotomy which showed a large, palpable, and polypoid mass in the distal stomach
A distal gastrectomy was performed because the intussusceptum was found to be necrotic. The patient’s recovery period after surgery was uneventful and was discharged 7 days after presentation. At 6-weeks follow-up, the patient did not have any complaints of vomiting and abdominal pain.
The lifetime risks of cancers combined may be as high as 93%, without proper medical surveillance. The syndrome is extremely rare with an estimated incidence of 1 in 8,300 and 1 in 280,000 live births. It is very rare for patients to present with bowel obstruction because of intussusception. Similarly, in this case, the diagnosis was unfortunately not made till the patient developed bowel obstruction because of an intussusception, for which the patient required laparoscopic bowel resection. Therefore, a high index of suspicion is needed for accurate diagnosis. Close surveillance and early identification can lead to excellent prognosis in the individuals.
References
Source: NEJM