Case of hemothorax during a challenging transseptal puncture
This article describes the case of a 76-year-old patient who developed hypotension after a challenging transseptal puncture which further led to a hemothorax. The patient’s medical history revealed that he had undergone a mitral valve port-access surgery for atrial tachycardia. However, after the procedure was completed, the patient was in hemorrhagic shock. Doctors then referred the patient for a CT angiography which showed a massive right hemothorax, though without active bleeding. The patient was referred for chest drainage and more than 2.5 litres of blood was evacuated. Similarly, despite the complication, the patient made full recovery.
Case study
Hypertension shortly after or during the removal of a catheter is an alert for possible anaphylaxis, haemorrhage or embolism in the air. In most cases, the patient may experience bleeding at the site of the catheter or within the pericardial cavity with cardiac tamponade. Meaning that the space around the heart fills with blood. This case highlights the possibility of hemothorax because of pericardial laceration. Thus, it should be included in the differential diagnosis. Pleural fluid can be detected on echocardiography and fluoroscopy during the procedure. In addition, compared to a CT scan, a lung ultrasound will help save time in detecting a large hemothorax. Identifying transseptal puncture is of pivotal importance. Helpful tools for diagnosing transseptal puncture include transseptal needles and intracardiac echocardiography.
In this case, a 76-year-old male patient presented to the emergency with no known allergies. The patient’s medical history revealed coronary artery disease, for which he underwent treatment and 3 stents were placed in the left anterior descending artery. In addition, the patient also had severe mitral valve prolapse with a dilated left atrium and atrial fibrillation. For treatment, the doctors advised the patient for a port-access mitral annuloplasty and surgical crypto-ablation, which the patient underwent in 2011. However, despite treatment, the patient developed atrial tachycardia and therefore, was referred for catheter ablation. The procedure was done under general anaesthesia. At the same time, vascular access was obtained via the femoral vein. In addition, a double transseptal puncture was done under TEE guidance and fluoroscopy. However, a minute after the puncture, the patient’s blood pressure dropped drastically to 70/40 mmHg. However, the TEE did not show any pericardial fluid.
Management
Doctors prescribed the patient intravenous fluids and intermittent phenylephrine with low dose norepinephrine. In addition, the doctors concluded that the hypotension was because of the anaesthetic drug and the procedure was not aborted. The patient further showed an atrial flutter with a cycle length of 230 ms. Several endocardiac mitral isthmus linear lesions and epicardial lesions were created from the coronary sinus, which helped the atrial flutter slow to a cycle length of 300 ms with a radiofrequency ablation catheter. However, the procedure could not have been prolonged because of ongoing hypotension. And a transmural block could not be achieved.
On arrival at the coronary care unit, the patient was conscious and did not complain of any pain. However, he was concerned because of the medical attention he was getting. Clinical examination was significant for pale lips and conjunctivae. There were no signs of hematoma in the groin area. All other examinations were within normal range, except for decreased breath sounds on the right side. There were no signs of distention in the jugular veins. The heart rate and sinus rhythm were within the normal range. Though blood pressure was 80/50 mmHg despite 3 litres of blood transfusion with crystalloid fluid.
Prognosis
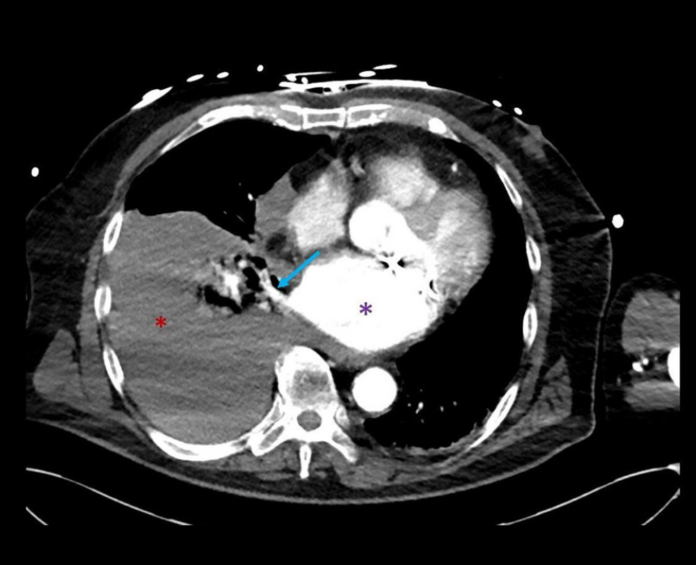
There were no signs of skin rash or wheezing. Doctors increased the dose of norepinephrine, and an urgent CT angiography was requested. They were concerned that the patient may have gone into hemorrhagic shock. The scans were significant for a massive hemothorax on the right side, consistent with recent blood loss. The patient was referred for chest tube drainage which evacuated more than 2 litres of blood in the first 24 hours, in addition to administration of two units of packed cells. The vasopressor drugs were tapered off and he did not require any thoracoscopic debridement of pleural blood. On follow-up only a small amount of pericardial fluid was present. The chest drain was removed 4 days after the procedure.
Hemothorax is a rare complication of catheter ablation and is usually caused because of and traumatic injury. However, in this case, the cause of the bleeding could not be established with certainty. As stated in the study, This bedside examination would have saved valuable time in establishing the diagnosis and avoiding the transport of an unstable patient to the CT scanner. Hemothorax is a collection of blood within the pleural cavity”.
Source: American Journal of Case Reports



