A 72-year-old Jehovah’s witness gets Hemopure to maintain her fatally declining haemoglobin levels.
This case describes the management of declining haemoglobin levels in a Jehovah’s witness with the use of Hemopure- investigational management. A 72-year-old female presented with failure to thrive and suspicion of aspiration pneumonia. The patient had a history of stage III nasopharyngeal melanoma. The tumour was resected followed by radiotherapy in 2011. The patient also had a history of follicular lymphoma status post-bendamustine. She was a Jehovah’s Witness.
After the radiotherapy to head and neck in 2011, the patient was suffering from difficulty in eating solids due to xerostomia and progressive dysphagia, therefore, she was on a liquid diet only.
Previous records and the current weight revealed a 25% weight loss over one year.
Serology revealed albumin of 2 g/dL, prealbumin of 4 mg/dL. Moreover, further tests confirmed the diagnosis of aspiration pneumonia.
Despite the oxygen mask, the patient’s saturation was dropping therefore her oxygen demands were increasing. Hence doctors transferred her to the intensive care unit. The patient had a septic shock on the 7th day of hospital admission.
The right femoral central venous catheter that the intensivist had placed lead to hematoma and pain around the insertion site, therefore they had to remove it. The hematoma was 2 × 3 cm i size. However, it remained stable over the next few days.
The patient required 35-40 L high flow nasal cannula. She experienced hypotension with diuresis. Moreover, her haemoglobin level dropped from 7.3 g/dL to 5 g/dL and the otherwise stable hematoma rapidly expanded overnight in right groin hematoma.
Ultrasound demonstrated a femoral pseudoaneurysm with an arteriovenous fistula between the superficial femoral artery and the common femoral vein.
The patient required vascular surgery. However, the patient’s haemoglobin was 4.5 g/dL before the surgery.
Postoperative Course:
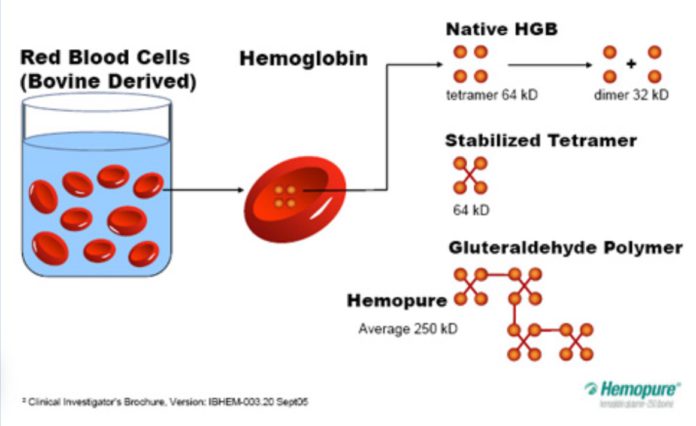
With the patient’s dropping haemoglobin level, she was given four units HemoPure, HBOC-201 as part of an investigational trial, over the next 24 hours after the surgery.
During transfusion of the first two units, the patient was also on epinephrine and vasopressin.
The doctors also gave her folic acid, cyanocobalamin, thiamine, erythropoietin, Vitamin C, and iron.
On the first postoperative day, she continued to require vasopressors. Her methemoglobinemia was 4.6%. The doctors transfused another two units. The patient no longer needed vasopressors, so all the vasopressors were weaned off during the next twelve hours.
After weaning, her fraction of inspired oxygen dropped from 100% to 65%. Her percent methemoglobinemia peaked at 8.6% on the second postoperative day. However, it returned to normal by the 7th postoperative day.
The doctors extubated her on the 3rd postoperative day.
Her haemoglobin improved to 5.7 g/dL and she maintained oxygen saturation on room air by the 9th postoperative day. She was able to be weaned to room air by postoperative day 9, therefore, the doctors shifted her to the ward.
From 16th postoperative day onwards till her discharge, her haemoglobin level remained between 9 and 10 g/dL.
Reference:
Nellis JR, Devinney MJ, Young CC (2020) Hemopure, HBOC-201, for Life Threatening Anemia in a Jehovah’s Witness. Int J Blood Res Disord 7:052. doi.org/10.23937/2469-5696/1410052