Granulomatosis with Polyangiitis Presenting with Ocular, Cutaneous, and Upper Airway Involvement in a Young Adult
Granulomatosis with polyangiitis (GPA) is a rare, systemic necrotizing vasculitis that predominantly affects small- to medium-sized vessels. It is classically associated with antineutrophil cytoplasmic antibodies (ANCAs), particularly proteinase 3 (PR3-ANCA). GPA typically involves the upper and lower respiratory tracts and kidneys, but it can present with diverse manifestations that may delay diagnosis, especially in young and previously healthy individuals. This article describes a case of granulomatosis with polyangitis presenting with ocular, cutaneous and upper airway involvement.
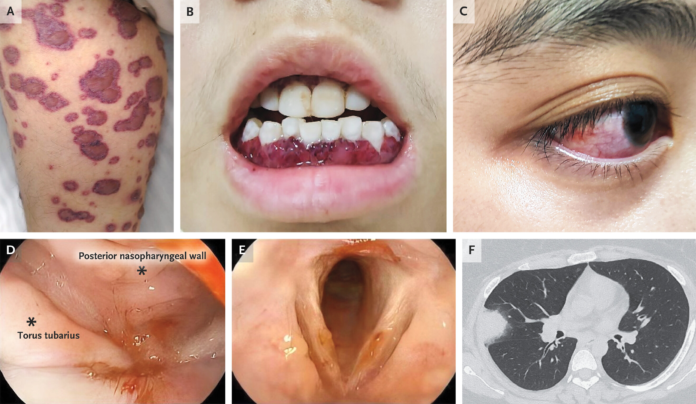
This case describes a 20-year-old woman who presented with a constellation of ophthalmologic, dermatologic, mucosal, pulmonary, and renal findings. Her initial symptoms included a 9-day history of right eye pain and decreased vision, along with a 2-week history of rash and gingival swelling. Ocular examination revealed scleral and conjunctival injection with a focal nodule, consistent with nodular scleritis, and funduscopic findings concerning for optic neuritis. Ocular involvement occurs in up to 50% of patients with GPA and may be the presenting feature; scleritis, episcleritis, and optic nerve involvement are well-recognized manifestations and can threaten vision if untreated.
Examination findings
Cutaneous examination revealed purpura with overlying vesicles and bullae on the chest, back, and legs. Skin involvement in GPA often reflects leukocytoclastic vasculitis and may present as palpable purpura, ulcers, vesiculobullous lesions, or nodules. These findings are indicative of systemic small-vessel inflammation and should prompt evaluation for systemic vasculitis.
Oral examination demonstrated dark-red, edematous gingiva with petechiae, a classic but uncommon finding known as “strawberry gingivitis.” This feature is highly suggestive of GPA and reflects granulomatous inflammation of the gingival mucosa. Although rare, strawberry gingivitis is considered relatively specific and can serve as an important diagnostic clue, particularly in younger patients without other comorbidities.
During hospitalization, the patient developed fever, dyspnea, and hemoptysis. Endoscopic evaluation revealed friable, hemorrhagic nasopharyngeal mucosa and ulcerated laryngeal tissue, consistent with upper airway involvement. GPA frequently affects the nasal cavity, sinuses, and larynx, leading to epistaxis, crusting, ulceration, and subglottic stenosis. Pulmonary involvement was confirmed by computed tomography, which demonstrated bilateral lung nodules. Pulmonary nodules, which may cavitate, are a hallmark of GPA and are often associated with hemoptysis.
Renal involvement was evidenced by proteinuria and hematuria on urinalysis, suggestive of a rapidly progressive glomerulonephritis. Renal disease is a major determinant of prognosis in GPA and often presents with minimal symptoms despite significant pathology. Serologic testing revealed a positive PR3-ANCA, supporting the diagnosis.
The patient was diagnosed with granulomatosis with polyangiitis and treated with pulse-dose intravenous methylprednisolone followed by cyclophosphamide and a tapering course of oral prednisone. Current guidelines support the use of high-dose glucocorticoids combined with either cyclophosphamide or rituximab for induction of remission in severe GPA. In this case, cyclophosphamide was selected due to clinical considerations. At 3-month follow-up, the patient showed substantial clinical improvement, underscoring the importance of early recognition and aggressive treatment.
This case highlights the protean manifestations of GPA and emphasizes the need for multidisciplinary evaluation when systemic inflammatory signs involve the eyes, skin, mucosa, lungs, and kidneys. Prompt diagnosis and treatment are critical to prevent irreversible organ damage and improve long-term outcomes.
References
- Jennette JC, Falk RJ. Pathogenesis of antineutrophil cytoplasmic autoantibody–mediated disease. Nat Rev Rheumatol. 2014;10(8):463–473.
- Hoffman GS, et al. Granulomatosis with polyangiitis: An analysis of 158 patients. Ann Intern Med. 1992;116(6):488–498.
- Pakrou N, et al. Ocular manifestations of granulomatosis with polyangiitis. Clin Exp Ophthalmol. 2006;34(6):557–565.
- Abdulahad WH, et al. Pathogenesis of ANCA-associated vasculitis: New insights. Autoimmun Rev. 2012;11(9):615–622.
- Yates M, et al. EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis. 2016;75(9):1583–1594.