Case Presentation
A 16-year-old Persian boy with no previous medical history presented with hip pain for the last 3 months. Physical activities triggered his pain, which gradually transitioned into continuous discomfort. While the pain wasn’t excruciating, it was moderate in intensity, impacting his ability to perform and even causing a noticeable limp.
Investigations
To find out the cause of the pain, doctors utilized magnetic resonance imaging (MRI) to visualize the hip joint. Given his discomfort and the presence of an abnormality near his upper thigh bone, close to the hip joint, as well as signal alterations detected by the MRI, the medical team recommended an initial biopsy. This was essential for an accurate diagnosis and effective management. The biopsy of the proximal femur specimen revealed a unique growth comprised of enlarged blood vessels with thin walls, intertwining with fibromuscular and bony tissues. The conclusion was “cavernous hemangioma of bone.” Supporting this, his laboratory blood tests showed normal levels of calcium, phosphate, albumin, and other indicators, reflecting a healthy bone metabolism.
Surgery
To alleviate the patient’s pain, the doctors made the decision to perform prophylactic fixation using a cephalomedullary nail. Despite the surgery, the patient’s pain persisted, even worsening to a severe level that landed him in the hospital’s emergency room just a month after surgery. An X-ray revealed a bone fracture and destruction, necessitating curettage, a structural fibula allograft, and fixation via a cephalomedullary nail. Fortunately, there was no post-surgery infection.
Recovery
Months later, doctors found a new set of concerns at a follow-up appointment. Bone density in the proximal femur was declining, and the transplanted allograft was being absorbed. This prompted a second incisional biopsy, which confirmed the recurrence of the cavernous hemangioma growth and, fortunately, the absence of malignancy. Based on this diagnosis, doctors deemed that the patient was a suitable candidate for sclerotherapy treatment.
Gorham Stout Disease
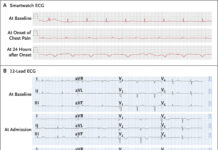
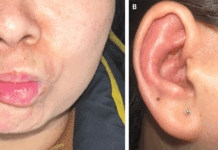
18 months after the initial biopsy, the patient’s situation led him to another medical center. The pain persisted, and his condition worsened. Upon his visit, he had intense pain, was bound to a wheelchair, and was fully disabled. Skin examination revealed surgical incisions as the only anomaly, and his ability to move was limited due to pain. While tests for inflammation and bone health appeared normal, the doctors further evaluated the patient due to his deteriorating condition.
Considering various factors—his age, laboratory results, the presence of lymphatic and vascular channel proliferation alongside bone trabeculae, the absence of abnormal cellular changes, and accompanying symptoms—the multidisciplinary team reached a conclusive diagnosis: Gorham Stout disease (GSD). Although doctors typically manage GSD by non-surgical treatments, the patient’s extreme pain and compromised mobility necessitate a more intricate approach. After long consideration, the doctors decided to go for the surgical approach. The surgery included the wide resection of the lesion and reconstruction employing the MUTARS® femoral system endoprosthesis.
Under general anaesthesia, they placed the patient in the supine position with a cushion supporting his right buttock. An incision was made in the skin, subcutaneous tissue, and fascia, exposing the bone through a lateral approach. The upper region displayed healthy muscles and soft tissues but an absence of bone tissue, with the previously inserted nail positioned between the muscles and firm tissue within the joint. Moving downward, the bone was fragile and soft. Given these findings, doctors made the decision to proceed with a total femur and hip joint replacement.
Doctors adjusted the prosthetic limb for length and rotation and reconstructed the ligamentous muscle connections. Once hemostasis was ensured and a drain inserted, the wound was systematically closed.
Doctors advised the patient to be in the abduction brace for 10 weeks along with a 14-month-long physiotherapy program, preceding additional medical treatment. After five years of regular follow-up, the patient regained his independence, although he still had a faint limp and occasional discomfort.
Gorham Stout Disease and Treatment
Gorham Stout disease (GSD) is a rare disease, with fewer than 400 documented cases in medical literature to date. Its typical appearance is in the late teens to early twenties, though instances have emerged in the younger and elderly age groups as well. While most studies indicate equal occurrence in both genders, some suggest a slightly higher prevalence in males.
The exact mechanism behind GSD remains elusive, although cellular and molecular studies have shown potential avenues. These studies propose an imbalance in bone metabolism. They are marked by increased bone resorption and insufficient regeneration, ultimately replaced by fibrous tissue. While most cases affect a single area, multiple sites can be involved, notably the spine and ribs. Frequently impacted regions include the spine, ribs, jawbone, shoulder, and pelvic girdle.
Treatment for GSD typically involves medical therapy, including calcium and vitamin D supplements, bisphosphonates, sirolimus, and interferon. Another management option for GSD is radiotherapy, often utilized as an adjunct therapy and reportedly effective.