Case Report
Eosinophilic fasciitis (EF) is a rare connective tissue illness, sometimes known as Shulman’s disease, whose cause and pathogenesis are unknown. Some studies suggest that severe activity or physical exertion prior to disease onset may be a significant cause. As well as nonspecific fascial inflammation and an immunological response to antigens released from the tissue. The disease’s clinical features include symmetric painful swelling and progressive sclerosis of the skin. And soft tissues of the extremities (excluding the hands and feet). As well as the appearance of orange-peel-like dimples and grooves on the skin in the advanced stages.
Peripheral blood eosinophilia, raised gamma globulin levels, and a higher erythrocyte sedimentation rate are common laboratory results. A complete biopsy, including fascia and muscle, proves the diagnosis of EF. Histological examination usually indicates subcutaneous connective tissue fibrosis, fascial thickening. And lymphocytic and plasma cell infiltration, with or without eosinophilic infiltration. Magnetic resonance imaging (MRI) can detect fascial edema and inflammation as it is indicative for the diagnosis of EF and shows noninferiority to a complete biopsy.
Corticosteroids are the current standard of care. As they are effective in more than 90% of patients, followed by methotrexate, cyclosporine, or cyclophosphamide if the steroid does not work. It is important to start the treatment right away to prevent residual sclerosis or joint contractures. As a result, once a definitive diagnosis has been established, therapy should begin immediately. We present a case with early EF that responded favorably to treatment.
Case Presentation
A 52-year-old Chinese woman presented with complaint of marked symmetrical edema in her limbs for two months, primarily impacting her forearms and calves. As well as reduced wrist and ankle joint mobility. Examination revealed severe symmetrical and circumferential swelling. And soreness on the backs of both hands, forearms, and calves, hardening of the skin on the flexed side of both wrists, and difficulty closing the palms of both hands.
This patient described a history of manual-intensive labor prior to symptom onset, with no previous treatment measures. Her medical history included 20 years of well-controlled hypertension using compound reserpine and triamterene pills. She denied having any allergies or a family history of rheumatic illnesses. The patient was a retired domestic servant.
Investigations:
Her initial lab results showed peripheral blood eosinophilia. Her eosinophil count remained stable for 3 months (from 1.37 × 109/L to 1.35 × 109/L. Additional testing revealed an increased immunoglobulin G (IgG) level. As well as serum interleukin 2R (IL-2R) and interleukin 17A (IL-17A) levels. The erythrocyte sedimentation rate (ESR) was increased, whereas CRP remained within normal range.
Antinuclear antibodies (ANA), anti-extractable nuclear antigen (ENA) antibodies, anti-phospholipid antibodies (APLA), and anti-neutrophil cytoplasmic antibodies (ANCA) all tested negative. There were no abnormalities in rheumatoid factor (RF), anti-citrullinated cyclic peptide (anti-CCP) antibodies, complement levels, muscle enzymes, or tumor serum indicator. And serum immunoglobulin electrophoresis and urine protein electrophoresis were normal. Chest CT and abdomen ultrasound indicated no inflammatory or neoplastic abnormalities. After completing the necessary examinations, infections with hepatitis and tuberculosis were excluded.
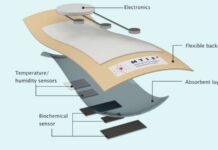
Later, the patient underwent enhanced magnetic resonance imaging (MRI) of both lower extremities and the right forearm prior to treatment. That revealed extensive edema in the intermuscular spaces and slight fascia thickening, as well as fascia. And tendon sheaths thickened in a ring-enhancement after enhancement by T1 lipid-suppressive sequences. A full-thickness fascia biopsy, which reached the fascia, was conducted on the subcutaneous tissue of the anterior side of her right calf. Histopathological investigation revealed fibrous tissue proliferation between subcutaneous fat lobules, interstitial edema. And perivascular lymphocyte and plasma cell infiltration, all of which are consistent with EF pathology. Additionally, immunohistochemical labeling revealed positive immunofluorescence for immunoglobulin M (IgM) in the deep dermal tissue between fat lobules.
This patient had symmetrical plate-like sclerotic and swelling lesions on all four limbs, but no Raynaud’s phenomenon or arthritis. Her lab results revealed peripheral blood eosinophilia. Although no eosinophilic infiltration was seen in the tissue. The histology of a skin biopsy that included the fascia revealed fibrosis of the subcutaneous connective tissue; concurrently, enhanced MRI revealed significant edema in the intermuscular space and fascial thickening with enhancement. As a result, the patient met the major and one of the minor criteria for the diagnosis of EF.
Treatment
The patient was started on intravenous methylprednisolone medication. It was switched to oral prednisone after 5 days, and methotrexate (MTX) as an immunomodulator. Within one week of starting therapy, the swelling and skin tension at the lesion site had subsided. And the patient could perform the closed palm test and walk without difficulty. Concurrently, serum eosinophil count normalized (0.08 × 109/L), and inflammatory indicators improved significantly. At the 1-month follow-up, edema in both wrists and calves had subsided, joint mobility had been restored, skin tension had decreased. And inflammatory markers were still within normal ranges.