Case of ectopic intrathyroidal thymic tissue in a 31-year-old patient
Ectopic intrathyroidal thymic tissue is a rare condition that often affects paediatric patients. But it is very rarely seen in adults. Doctors often discover the condition incidentally on cervical imaging. However, it is also often misdiagnosed as benign or malignant thyroid lesions such as nodules or malignancies. This uncommon condition is frequently observed during the prepubertal period when the thymus is at its fastest growth stage and the massive thymus within the thyroid becomes visible. Later, as adults, the thymus undergoes a process known as involution, in which adipose tissue replaces the thymic tissue. As a result, adult diagnosis of persistent thymic tissue within or outside the thyroid is extremely rare.
Case presentation
This article describes the case of a 31-year-old Persian female patient with a history of a mass on the left side of the neck with a history of 1 year. On her referral to the clinic, the patient was in her second trimester, had two children and worked as a high school teacher. The patient had no history of smoking, drinking, or using drugs. Furthermore, her medical history was not significant for hyperthyroidism or hypothyroidism or constitutional symptoms in the patient. A history of diabetes mellitus, hypertension, and hyperlipidemia were also negative in this case. There was no significant past medical history or family history of ectopic cervical masses or thyroid gland lesions in the patient. The patient was currently not taking any medications.
Investigations and diagnosis
At the time of admission, the vital signs were normal, with a blood pressure of 120/80 mmHg, a pulse rate of 85 beats per minute, and a temperature of 37 °C. The primary examination of all 12 cranial nerves revealed no abnormalities. A palpable firm mass without tenderness was found in the left lobe of the thyroid during a neck examination. There was no bruit detected during thyroid auscultation. Thyroid function tests revealed that the patient was euthyroid (thyroid stimulating hormone 1.5 mIU/L, free T4 = 1.1 ng/dL, T3 = 150 ng/dL). WBC = 8000/mL, haemoglobin = 12 g/dL, hematocrit = 40%, platelets = 250,000/mL, alanine aminotransferase = 20 units/L, aspartate aminotransferase = 10 units/L, alkaline phosphatase = 60 IU/L, urine analysis = normal, urine culture = no growth).
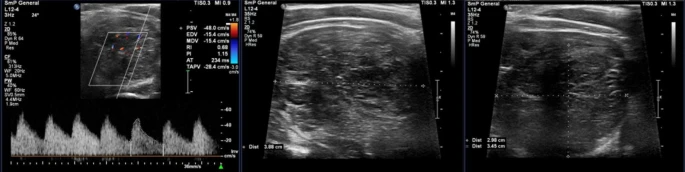
A hypo- to isoechoic nodule with internal striation and cystic areas was found in the lower pole of the thyroid gland’s left lobe during a neck and thyroid ultrasound. The examination revealed no micro- or macrocalcification in the lesion. The US investigation found no evidence of cervical lymphadenopathy. The lesion was fine needle aspirated (FNA). Moreover, the microscopic examination of prepared slides revealed numerous lymphoid cells of various sizes, including some atypical large lymphoid cells with a high nuclear-to-cytoplasmic (N/C) ratio and prominent nucleoli. The cytopathology of the specimen revealed tissue that was suspicious of lymphoproliferative disorder, and an excisional biopsy of the mass was advised. Furthermore, the patient underwent total thyroidectomy for surgical excision of the lesion, and postoperative pathology revealed thymic tissue.
Follow-up
The patient was referred for reevaluation six months after surgery. All physical examinations and laboratory tests were rechecked and found to be normal.
Hematoxylin and eosin (H&E)-stained sections of the excised lesion revealed an encapsulated mass with a thick fibrous capsule and intersecting fibrous bands separating it into lobulated architecture with cellular lobules resembling normal thymic cortex, composed of scattered bland thymic epithelial cells in a dense background of small lymphocytes (immature T cells). The immunohistochemistry (IHC) analysis revealed immunoreactivity for cytokeratin AE1/AE3 (CK AE1/AE3) and P63 in the scattered epithelial tumoral cells.
Source: Journal of Medical Case Reports