Case of dapsone-induced severe agranulocytosis in 7-year-old Sri Lankan girl with borderline leprosy, causing life-threatening skin sepsis.
This article describes the case of a 7-year-old Sri Lankan girl with borderline leprosy, diagnosed with dapsone-induced severe agranulocytosis which caused a life-threatening skin sepsis. The patient presented with a 2-day history of fever and swelling of the face. The symptoms gradually progressed causing dysphagia and difficulty in breathing. Examination was remarkable of an ill, febrile child with notable swelling of the face and neck associated with cellulitis.
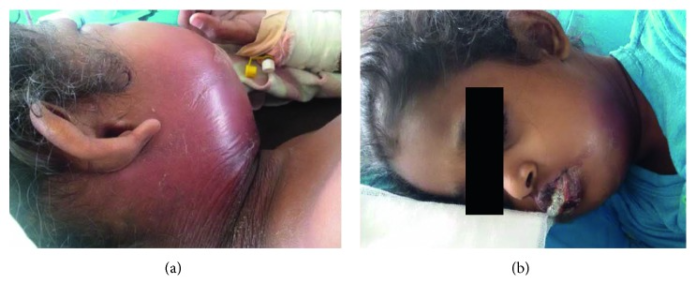
The patient’s clinical condition deteriorated with severe cellulitis and deep-seated abscess formation in the submandibular region, resulting in stridor. In addition, two hypopigmented skin lesions were also notable over her left arm. Physical examination further showed loss of thermal sensations, raising the suspicion of leprosy. There were no signs of thickened palpable nerves. Her medical history revealed that the child had been on rifampicin and dapsone for 2 months. Although, there was no monitoring of cell counts since the commencement of anti-leprosy medication.
Investigations
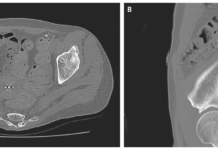
Laboratory reports showed a white blood cell (WBC) count of 1,000/mm3 with an absolute neutrophil count (ANC) of zero. Her blood picture revealed dapsone-induced changes with agranulocytosis, blister cells and numerous bite cells. However, doctors advised against bone marrow examination because the child showed improvement with supportive care. Blood culture was sterile, whereas liver and renal functions were also normal. Additionally, serial USS was remarkable of deep-seated abscesses in the submandibular region with overlying skin oedema.
Initial treatment included immediate cessation of dapsone with initiation of broad-spectrum antibiotics. The abscess was drained with repeated incision and drainage. In addition, the stridor and airway compression were managed with nebulised adrenaline and IV dexamethasone. However, the patient poorly responded to granulocyte colony-stimulating factor (GCSF) for management of neutropenia. Therefore, management of neutropenia was alternated with buffy coat transfusion.
The patient showed complete recovery after 5 days of admission.
References
A Case of Dapsone-Induced Severe Agranulocytosis Causing Life-Threatening Skin Sepsis in a Sri Lankan Child with Borderline Leprosy: A Success Story! https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6526580/