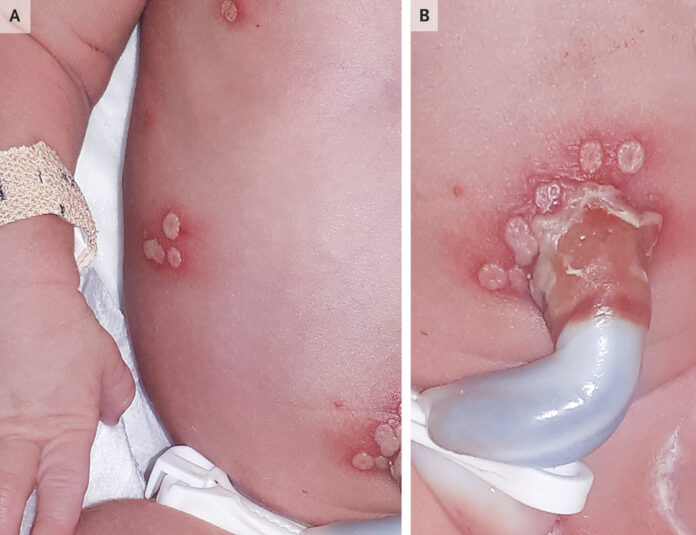
Neonatal herpes simplex virus infection post-delivery at 32 weeks’ gestation
After a spontaneous vaginal delivery at 32 weeks’ gestation, a baby girl was found to have vesicular skin lesions. Twelve days prior to the delivery, her 37-year-old mother’s membranes prematurely ruptured. Clusters of vesicles were discovered during a physical examination on the infant’s chest (Panel A), periumbilical area (Panel B), pharyngeal, nasal, and conjunctival mucosa. Both the placenta and the mother’s genitalia were free of lesions. Herpes simplex virus type 1 (HSV-1) was detected by polymerase-chain reaction (PCR) testing on samples taken from the infant’s skin, eye, throat, and blood. The patient was given the diagnosis of neonatal herpes simplex virus.
The findings of the liver biochemistry testing, lumbar puncture, and chest radiography were all normal. Neonatal HSV-1 infection limited to the skin, eyes, and mucosa was identified as the cause. The mother stated that she had never previously been infected with HSV-1. A postpartum endocervical PCR experiment, however, revealed the presence of HSV-1. In this instance, it was believed that a primary maternal infection acquired late in pregnancy caused an ascending intrauterine infection, which may have caused preterm labour following a protracted membrane rupture. Acyclovir treatment was provided. The youngster had no recurrences and was developing normally at the age of 2.
Herpes Simplex Virus infection in Neonates
Infants with herpes simplex virus (HSV) infection may have the following symptoms: organs affected by disseminated disease, with the liver and lungs most commonly involved (25%); Skin involvement or localised central nervous system (CNS) disease (30%); and SEM disease (disease confined to the skin, eyes, and/or mouth) (45%). Skin vesicles are present in more than 80% of newborns with SEM illness. Patients without skin vesicles have an infection that is only present in their eyes or mouth mucosa. When neonates exhibit symptoms of sepsis syndrome, negative results from bacteriologic cultures, significant liver failure, or consumptive coagulopathy, widespread infection should be taken into account.
Although the first symptoms of HSV infection can appear at any time between birth and six weeks of age, the majority of infected infants show clinical symptoms within the first month after birth. Infants with disseminated disease and SEM disease often present between the first and second weeks of life, which is an early age of onset. Between their second and third weeks of life, infants with CNS diseases typically begin to show symptoms of sickness.
Epidemiology
1 in 3000 to 1 in 20,000 live births are estimated to be affected by neonatal HSV infection. Although it can be brought on by an ascending infection through ruptured or unbroken amniotic membranes, HSV is most commonly transmitted to a neonate during birth through an infected maternal genital tract. Postnatal transmission by a parent or other carer, typically from a non-genital lesion, such as on the mouth or hands, is another, less frequent source of neonatal infection.
Studies have shown that a mother who contracts primary genital infection close to birth runs a 25% to 60% risk of transmitting HSV to the unborn child. However, the chance of a mother reactivating an infection she had in the first trimester of pregnancy or earlier and passing it on to her unborn child is less than 2%. Because primary and recurrent genital infections may be asymptomatic or linked to nonspecific symptoms (such vaginal discharge, genital discomfort, or shallow ulcers), differentiating between primary and recurrent HSV infections in women by history or physical examination alone may be impossible.
Since more than 75% of infants with HSV infection are born to women who have no history of genital HSV infection or clinical findings suggesting genital HSV infection during or prior to pregnancy and who are therefore unaware of their infection, the history of maternal genital HSV infection is not helpful in diagnosing neonatal HSV disease.
Source: NEJM