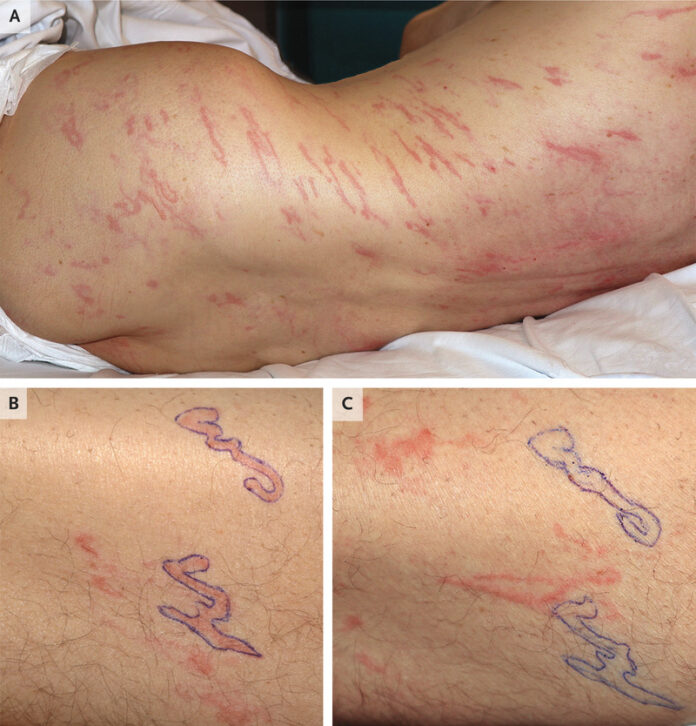
Larva Currens in Strongyloides hyperinfection Syndrome
This article describes the case of a 64-year-old man with metastatic adenocarcinoma diagnosed with larva currens, a manifestation of Strongyloides hyperinfection syndrome. The patient developed an itchy rash and mild diarrhoea when he was hospitalised for malignant spinal cord compression. لعب لربح المال Doctors had started the patient on high-dose glucocorticoid therapy 4 days before the symptoms had started. The patient’s medical history revealed that he suffered from peripheral eosinophilia of an unknown cause 3 years ago. His maximal absolute eosinophil count was significantly increased. He lived in an urban region of Spain all his life and worked as a sewage manager. العاب مجانية عبر الانترنت The examination was significant for raised, erythematous serpiginous tracts. The lesion had originated in the perianal area and had spread to the trunk and limbs. The lesions were outlined with a pen and reevaluated 24 hours later. It was found that after 24 hours, the lesions had migrated from their original location.
Stool examination was significant for rhabditiform and filariform larvae of species Strongyloides stercoralis. Based on these findings, doctors diagnosed the patient with Strongyloides hyperinfection syndrome with larva currens. Larva currens is characterized by an urticarial rash that is caused by the subcutaneous migration of flariform larvae during a part of their life cycle. The migration of the larvae is accelerated in Strongyloides hyperinfection syndrome. Treatment included oral ivermectin after which the patient’s rash and diarrhea abated [1].
Strongyloidiasis hyperinfection syndrome
Strongyloidiasis is an intestinal infection that is caused by two species of parasitic nematode Strongyloides. The most clinically important and common pathogenic species in humans is S stercoralis. A distinctive characteristic of this species is its ability to persist and replicate within a host with minimal or no symptoms for decades. However, it can cause life-threatening infections, for example, hyperinfection syndrome and disseminated strongyloidiasis) in immune-compromised individuals.
The true prevalence of the disease is often overlooked because the infection is subclinical in most cases. The infection is uncommon in the United States but is endemic in the rural areas of southeastern states and the Applachia region and has a prevalence rate of 4%. Additionally, strongyloidiasis is more prevalent in patients in long-term institutionalised care, such as in mental health facilities and prisons, immigrants or refugees from tropical and subtropical regions and in people who were stationed in the Vietnam War or Southeast Asia during World War II.
Another study conducted in Washington, DC showed that Southeast Asians had the highest incidence of infection [2]. An epidemiological study conducted in Canada showed similar findings, the infection was reported in 11.8% of the Vietnamese population, whereas 76.6% of Cambodian immigrants were positive for the infection [2]. Studies have shown that the infections acquired in the U.S. are generally not associated with larva currens.
International statistics
The prevalence of strongyloidiasis was estimated to be 8.1% in 2017, which equals to 613.9 million people. The global prevalence is, however, 10 times higher than the previous estimate, between 30 to 100 million people. The highest number of infected people is in the Southeast Asia region. Whereas the global prevalence is as high as 40% in some areas including West Africa, the Caribbean and Southeast Asia due to the moist soil and improper disposal of human waste. The infection is also commonly seen in Colombia, temperate regions of Spain, Brazil, Cuba and Panama. روليت However, the highest rates of larva currens are reported in Latin America. “The international prevalence of larva currens among patients with strongyloidiasis varies, with rates in the range of 30% to 90% in Southeast Asia. High rates of larva currens are also reported in Latin America. A stool and serosurvey for S stercoralis conducted in a community in the Peruvian Amazon region found strongyloidiasis due to S stercoralis in the stool of 69 (8.7%) of 792 participants” [2].
Racial and age difference
There is no racial predilection apparent for Strongyloides infection. However, as mentioned above, Southeast Asia has the highest endemic percentage of Strongyloides infection. Larva currens is most frequently seen in white patients who have acquired the infection from Southeast Asia. Similarly, while it is common in all ages, the infection occurs more frequently in children because they are more likely to play outdoors in contaminated soil with bare feet. Increasing age is also a risk factor for severe strongyloidiasis since it may be associated with an immunosuppressive state.
Sources



