Case of COVID-19 myocarditis in a 23-year-old male
COVID-19 has been associated with different degrees of cardiovascular involvement, with myocarditis as one of the feared complications. However, despite an increase in the number of cases with a cardiovascular presentation, there is a lack of data on the management and prognosis of myocarditis. In addition, there is not enough information on myocardial scarring post-acute COVID-19. In a similar case, a 23-year-old male patient presented to the outpatient cardiology clinic 10 months post COVID-19 with persistent myocardial involvement.
Case report
This article describes the case of a 23-year-old male patient who presented to the outpatient cardiology department with a 1-week history of left-sided chest discomfort. According to the patient, the discomfort would last for 30 to 60 minutes before resolving. The patient’s history further revealed that he would run for 2 miles a day, 6 days a week without any issues. However, 3 months before presenting to the department, the patient was diagnosed with COVID-19 which was managed without any issues. In addition to this, the patient’s medical, surgical and social history did not show any significant findings.
On physical examination, there were no signs of fatigue. In addition, vital signs were also within a normal range. There were no signs of cardiopulmonary abnormalities either. Doctors further referred the patient for laboratory evaluation. Findings of the laboratory test showed normal serum troponin levels and B-type natriuretic peptide. The patient was also referred for an EKG which showed bradycardia and an incomplete right bundle branch block. In addition, the transthoracic echocardiogram showed a left ventricular ejection fraction of 60%, however, with no signs of valvular or wall motion abnormalities. Based on the patient’s current symptoms and positive COVID-19 PCR, the doctors evaluated the patient for possible myocarditis. The patient was further referred for TTE which showed a left ventricular ejection fraction (LVEF) of 60%, however, with no signs of motion abnormalities.
Based on the patient’s symptoms and COVID-19 diagnosis, he was further referred for evaluation of myocarditis
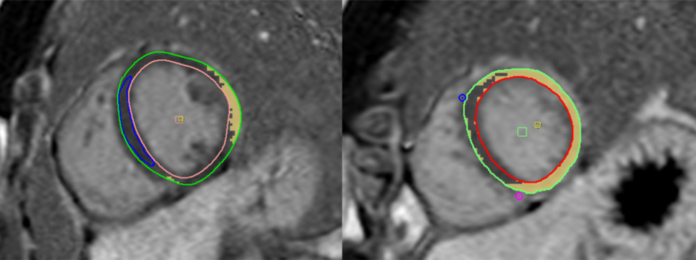
The patient was advised cardiac magnetic resonance imaging for evaluation of myocarditis. In addition, doctors referred the patient for various imaging sequences including steady-state free precession, along with tissue characterization using T2 map images and LGE images using sensitive inversion recovery (PSIR). CMR findings were significant for a mildly dilated right atrium. However, the cardiac chambers were normal-sized. The findings were significant for a left ventricular ejection fraction of 54% with signs of trace pericardial effusion. The global native T1 and T2 values were within the normal range, this finding is consistent with the diagnosis of no myocardial oedema.
However, the LGE images showed the presence of several areas of sub-epicardial and pericardial enhancement. Based on these findings the patient was diagnosed with myopericarditis. The patient was started on colchicine (medication used for the treatment of gout and Behcet’s disease) for 3 months and ibuprofen for 14 days. The patient was called back for a follow-up a month later. Examination showed that the patient’s symptoms had resolved. A treadmill stress test was performed which showed a good exercise capacity and there were no signs of abnormalities on the EKG. CMR was repeated 7 months after the initial presentation. The findings showed persistent sub-epicardial fibrosis in the same area the myopericarditis was detected earlier. Although there were signs of improvement in the LGE burden by 5.1% with resolution of pericarditis.
Cardiovascular implications of COVID-19
The cardiovascular implications of COVID-19 include myocarditis, coronary artery disease, postural orthostatic tachycardia syndrome, arrhythmias and pericarditis. CMR, as of recently is being utilised for a wide range of COVID-19 patients with cardiac concerns. The concerns may either be asymptomatic or signalling severe disease. Myocarditis is diagnosed using the Lake Louis and modified Lake Louis criteria. However, in subacute settings, tissue oedema and scarring are diagnostic features for myocarditis. Studies have further shown that the presence of LGE is present for up to 6 months in non-ischemic patients post COVID-19 infection. However, the implications of this myocardial scarring are yet to be elucidated.
The presence of myocarditis is an alarming concern in young and healthy individuals post-COVID as it may represent an undetected myocardial involvement with potential future consequences. Though, only 11% of the patients show complete resolution of myocarditis in symptomatic acute COVID-19 at a 6-month follow-up. Patients with LGE are at an increased risk of major cardiac events, including heart failure hospitalizations, shock and cardiac arrest. Whereas patients with increased LGE have a poorer prognosis.
Source: American Journal of Case Reports



