Case Report
Primary malignant cardiac endosarcoma are exceptionally rare. According to the 2021 World Health Organization (WHO) categorization of cardiac tumors, the majority of initial heart tumors are benign. Papillary fibroelastoma (PFE) has become the most common benign tumor, appearing roughly twice as frequently as myxomas. Malignant tumors make up less than 10% of all primary cardiac tumors, with cardiac angiosarcoma (AS), undifferentiated pleomorphic sarcoma (UPS), and cardiac leiomyosarcoma (LMS) being the most common subtypes, accounting for roughly three-quarters of all cardiac sarcomas.
Cardiac AS and UPS each account for approximately one-third of occurrences. These sarcomas usually emerge between the fourth and sixth decades of life. The UPS and LMS primarily occur in the left atrium with no sex preference, whereas AS disproportionately affects males and prefers the right atrium. Cardiac tumor symptoms are typically nonspecific, necessitating a high level of suspicion for diagnosis. Patients typically report nonspecific symptoms such as chest discomfort, dyspnea, weight loss, and malaise, which might delay diagnosis. Of all cardiac sarcomas, AS has the poorest prognosis, with a 5-year overall survival rate of about 10%.
Case Presentation
A 48-year-old previously healthy Han Chinese woman with no notable medical history presented with a 2-week history of exertional chest tightness and dyspnea, which deteriorated and was accompanied by hemoptysis. A physical examination found no significant abnormalities. The patient has no history of long-term pharmaceutical usage, no family history of genetic illnesses, and was previously physically and psychologically fit.
Investigation:
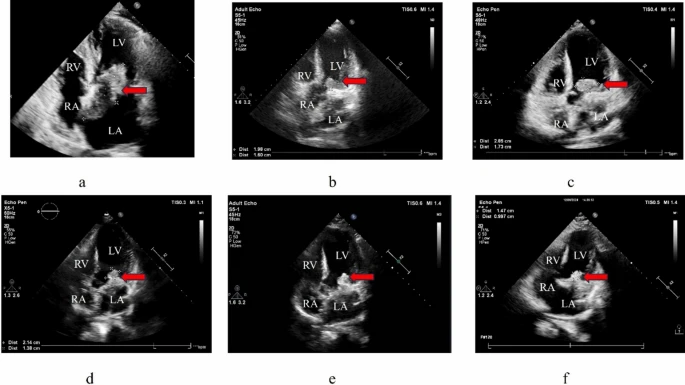
The transthoracic real-time three-dimensional echocardiography revealed an irregularly shaped, isoechoic mass in the left atrium of approximately 64 × 41 mm. The tumor was connected to both the interatrial septum and the base of the mitral valve annulus. It had well-defined borders and unequal internal echogenicity, with parts of the mass shifting between the left atrium and the left ventricle throughout the cardiac cycle. Contrast-enhanced chest CT revealed a hypodense lesion in the left atrium (54 × 43 mm) with septations and modest elevation, partially extending into the left ventricle. Upon admission, tumor markers carcinoembryonic antigen (CEA) (10.48 ng/mL), neuron-specific enolase (NSE) (38.71 ng/mL), and cancer antigen 125 (CA125) (182.97 U/mL) were all elevated.
Management
The patient had cardiac tumor excision with temporary pacemaker insertion while on cardiopulmonary bypass. In January 2024, the patient had general anesthesia and cardiopulmonary bypass for “cardiac tumor resection + temporary cardiac pacemaker lead implantation”. Intraoperative examinations revealed left atrial enlargement, and a portion of the interatrial septum was removed along the tumor boundary. The tumor, measuring about 4 × 5 cm, was hard and infiltrative. It was located in the left atrium and protruded into the right atrium. Its base was linked to the interatrial septum and invaded the endocardium. A gelatinous and friable tumor mass (~3 cm) was seen around the mitral annulus.
Subendocardial bleeding was also observed in the left atrium. Following removal, the mitral valve showed slightly regurgitant but not stenotic. Intraoperative observations were left atrial enlargement and a hard, infiltrating tumor measuring 4 × 5 cm. Histopathological examination revealed a spindle cell sarcoma of mesenchymal origin with an immunohistochemical profile similar to intimal sarcoma. The diagnosis is primary cardiac endosarcoma.
Post Operative Period
The procedure went smoothly, and the patient made a full recovery after more than two weeks in the hospital. Symptoms such as chest tightness and dyspnea were relieved after surgery. A recurrence occurred 31 days after surgery, and echocardiography detected a mass in the left ventricle (19.8 × 16 mm). Genetic tests found amplification of the MDM2 gene, which is typically linked to sarcomas. Given the disease’s fast clinical progress, the patient was started on liposomal doxorubicin at a dose of 40 mg, delivered as a 16-hour continuous intravenous infusion using an electronic pump. The treatment protocol was repeated every 21 days. The patient underwent three cycles of liposomal doxorubicin as first-line treatment.
After three cycles of treatment, follow-up echocardiography revealed a mass growth to 28.5 × 17.3 mm. The patient experienced leukopenia and fatigue during chemotherapy, improved with granulocyte colony-stimulating factor (G-CSF). Subsequently, anlotinib (10 mg daily) was given, leading to a reduction in mass size to 21.4 × 13.8 mm over several months, without notable adverse reactions. By November 2024, echocardiography indicated tumor progression with enlargement of the left atrium and ventricle, plus new mass-like lesions around the mitral valve orifice, measuring approximately 24 × 22 mm.
At the latest follow-up, a patient experiencing exertional chest tightness and dyspnea was treated with a regimen of gemcitabine, docetaxel, and anlotinib. This treatment resulted in a notable reduction in mass size after two cycles, with no new adverse events reported. The patient remains stable more than 1 year post-presentation, maintaining good physical function (NYHA class I–II) and regular follow-up, without signs of heart failure or arrhythmia. Radiotherapy was not used during the treatment period.