Autoimmune limbic encephalitis, a common presentation for hospital admissions.
This article describes the case of a 47-year-old female patient with a history of chronic pain syndrome and rheumatoid encephalitis diagnosed with autoimmune limbic encephalitis. The patient presented to the hospital with gait instability, increase somnolence, slurred speech, short-term memory loss and intermittent episodes of confusion with a history of 2 weeks.
A complete examination showed pain at multiple locations, minor falls and intermittent dizziness. She was currently taking medications including diclofenac, tramadol, folic acid, golimumab and methotrexate for pain. The patient’s family history further revealed a family history of coronary artery disease. She was a nonsmoker and denied using any illicit drugs or alcohol. She worked as a cashier. Her physical examination showed an unremarkable abdominal, lung and heart exam. There was mild swelling in both her wrists, however, with no signs of bony deformities. She had good personal hygiene with normal vital signs.
Examination findings
There were no signs of rash on skin examination. Neurological exam showed a motor strength of 5/5 in her extremities. Although, there were limitations in her left wrist because of pain. Similarly, sensations to light touch, vibrations and pinprick were normal and symmetrical. There were no tremors or asterixis or clonus. Neurological exam showed normal level of alertness, poor insight, circumstantial thought process, intermittent slurring of speech, flat affect, good eye contact and cooperative behaviour, also.
Laboratory examination showed no significant findings either except for hyponatremia. The patient’s serum pregnancy test was also negative. CT scan did no show any evidence of intracranial haemorrhage. Doctors further advised an MRI of the brain and cervical spine which also did not show any obvious abnormalities other than minimal cervical spondylosis at C4 and C6 levels.
The patient had initially presented to the hospital for altered mental status.
Doctors started the patient on fluid restriction and urea tablets. In addition, stopped her current medications. On the 2nd day at the hospital, the patient showed twitching of the upper right extremity in the absence of focal neurological deficits. On interrogation, the patient could not recall any of the events from the previous day. For this reason, doctors referred her for a neurological consultation. The neurologist put her on levetiracetam and placed on a 48-hour video EEG monitoring. 12 hours into the treatment, she showed generalised slowing of the background waves and left-sided periodic lateralised epileptiform discharges (PLEDs).
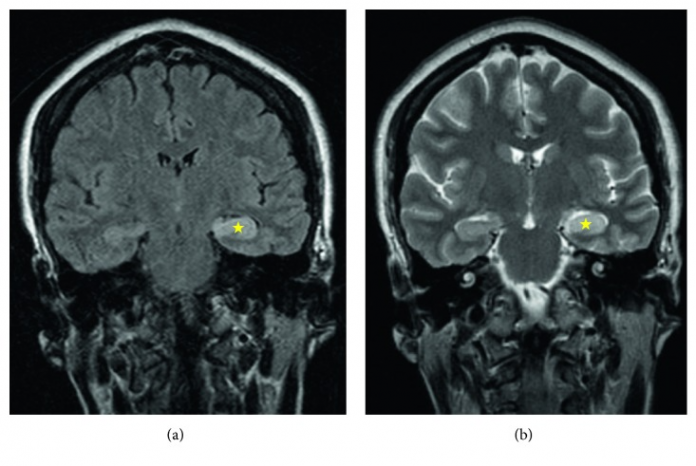
Lumbar puncture was remarkable for a high IgG index and minimally elevated opening pressure. However, because of a lack of improvement in the patient’s clinical status, doctors advised repeating the brain MRI. The MRI showed T2 hyperintensity with mild swelling of the left hippocampus in the presence of abnormal contrast enhancement. The findings led to the diagnosis of autoimmune limbic encephalitis, an inflammatory etiology for her neurological abnormalities.
Doctors treated her with 1 g methylprednisolone. CT of her head, neck, chest, abdomen and pelvis were negative for any tumours. The patient did not show any improvement, therefore, treatment was alternated with intravenous immunoglobulin (IVIg). She was discharged with close outpatient neurology follow-up.
References
Autoimmune Limbic Encephalitis in a Patient with Acute Encephalopathy and Hyponatremia https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6800970/



