Choriocarcinoma is an hCG producing tumour, which is seen in the setting of GTD (gestational trophoblastic disease). The tumour entails a group of benign hydatidiform mole and malignant invasive mole, choriocarcinoma, and other tumours arising from the placenta or uterus. Moreover, choriocarcinoma represents less than 5% of GTDs and has an association with very high hCG concentration. There is also a probability of hyperthyroidism due to cross-reactivity with the TSH receptor. The prognosis of GTD is usually excellent and it has a good response to effective chemotherapy with long term survival. But high risk malignant GTD has an overall 5-year survival rate.
Choriocarcinoma is very uncommon in extragonadal sites with PGC (primary gastric choriocarcinoma), which represents 0.08% of all gastric cancers. Although it has a poor prognosis, and this case is a presentation of a patient with PCG presenting with thyrotoxicosis.
Case Presentation
A 62-year-old Hispanic woman, previously healthy, with two spontaneous abortions had a three-week history of shortness of breath, palpitations, new onset of hot flashes and pain in her right flank.
Doctors did a physical examination, which revealed tachycardia and her speech compromised due to shortness of breath. Moreover, her conjunctiva was pale with no erythema, exophthalmos, and chemosis. Palpation of the thyroid gland showed no abnormalities. However, the sound of her heart increased in frequency with a systolic tricuspid murmur. In addition, there was a decrease in her basal breath sound on auscultation. Palpation of the liver revealed hepatomegaly, in addition, the area was hard, and tender along with hyperlexia and tremor. They also did a chest x-ray, which was normal and a renal ultrasound revealing multiple nodules in the liver.
Evaluation and Management
The doctors referred her for further evaluation and management. They did some laboratory tests, which were significant for normocytic anaemia, elevation in alkaline phosphate, elevation in lactate dehydrogenase, T4 elevation with suppression in TSH, consistent with thyrotoxicosis.
An echocardiogram showed pulmonary hypertension, in addition to dilation in the right atrium and ventricle. Moreover, ECG also revealed, adequate left ejection fraction, tricuspid regurgitation, atrial septal defect (previously unknown), interarticular communication with the right to left shunt along with a high risk of embolism.
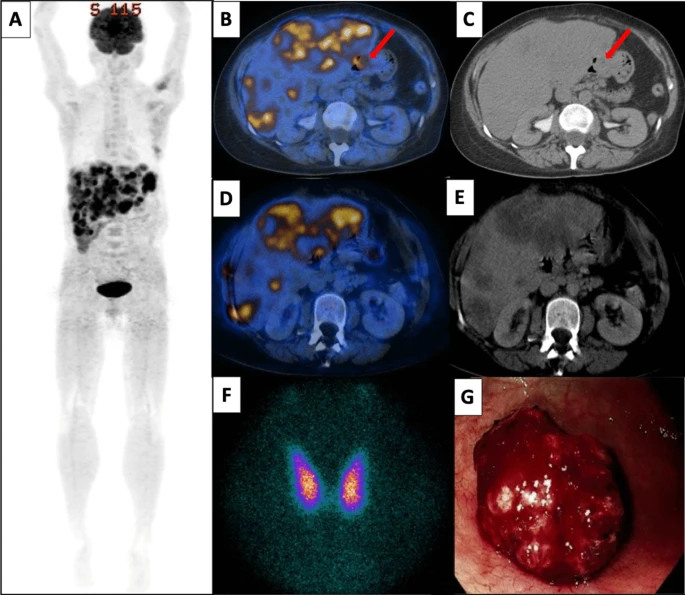
Doctors also did a contrast-enhanced FDG PET-CT, which revealed hepatomegaly and multiple large masses of the liver that were FGD-avid. Moreover, her doctors also saw a focus on FDG avidity in the stomach without any structural correlation.
Moreover, her thyroid scans were consistent with thyrotoxicosis; this was due to hyperthyroidism. Since the doctors saw no sign of Graves orbitopathy, they ruled out Graves’ disease. There was no goitre and a negative thyroid-stimulating body. Other than her test results, during the presentation, she had mildly altered liver function tests.
Treatment and Further Investigations
The doctors started her on propofol and antithyroid drugs. After stabilization of thyrotoxicosis, doctors did the upper endoscopy. It revealed a lesion that was bleeding in the greater stomach curvature. The gastric biopsy was consistent with choriocarcinoma. In addition, there was evidence of extensive necrosis with no evidence of concurrent conventional adenocarcinoma. No endodermal sinus component was present either. Immunostaining for antibodies was positive. In addition, the neoplastic cells had a diffuse and strong membranous reactivity to the antibody.
There was an extreme elevation in the beta-human chronic gonadotropin hormone subsequently. Furthermore, other markers of tumour measured were unrevealing. Once all the workup was done by the doctors, an extragonadal geminal tumour known as primary gastric choriocarcinoma in addition to liver metastasis and paraneoplastic hyperthyroidism was the suggested and most likely diagnosis.
The doctors treated the patient with methotrexate and subsequent treatment included etoposide in addition to cisplatin. They also titrated down the methimazole from 30mg to 10mg per day. This helped them in achieving euthyroidism. The antithyroid drugs along with the concurrent chemotherapy actively controlled the thyrotoxicosis.
Readmission and Prognosis
A month after the initial diagnosis, the patient came to the hospital again and was readmitted with hemorrhagic hypovolemic shock. This was due to a bleed in the GI in addition to acute liver failure and severe coagulopathy. The doctors discontinued the methimazole due to the onset of liver failure. She was given intensive care therapies with the help of a multidisciplinary team. However, she died a month and a half after the presentation due to multiple organ failures.
Conclusion: Severe Thyrotoxicosis in Metastatic Choriocarcinoma
Severe thyrotoxicosis can have an unusual presentation initially. It is usually presented by metastatic choriocarcinoma when there is an extreme elevation of beta-human gonadotropin. However, the outcome of primary gastric choriocarcinoma is very poor because it is an aggressive malignancy. Moreover, when there is a co-occurrence of severe aggressive thyrotoxicosis in addition to advanced primary gastric choriocarcinoma and imminent live failure, the management options become very complicated.