- Temporomandibular joint reconstruction is a challenging clinical problem, however, has been revolutionised with he development of total alloplastic TMJ replacement.
- However, because of high costs, an alternative approach is used to treat comminuted mandibular condyle fracture.
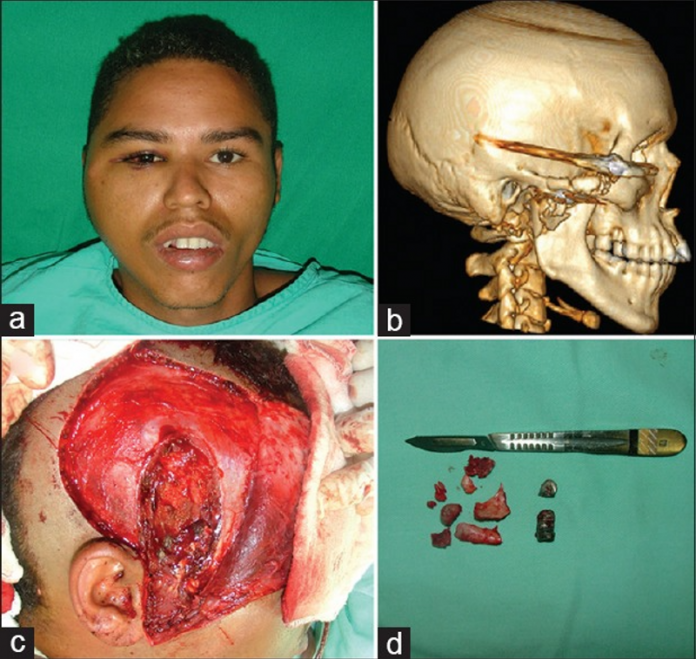
A 19-year-old male patient presented to the emergency department with a gunshot wound behind his ear after a robbery. Physical examination showed a right comminuted condylar base process and zygomatic arch fractures.
The patient required immediate treatment to prevent infection at the site. Moreover, treatment plan included a surgical procedure with an extended periauricular incision, removal of the proximal and fractures bone fragments, including condylar head, removal of foreign bodies, reshaping and flattening of the distal segment fractured surface, if viable, fixation of the remaining disc with a 2-0 nylon suture inserted posteriorly and laterally to the condyle neck anchored to two 2.0 mm screws. In addition, lining of the temporoandibular joint with temporalis fascia of Erich arch bars and early elastic therapy.
Follow-up after surgery
After the procedure the patient showed good mandibular motions (>35 mm), satisfactory occlusion with maximum intercuspation of teeth. However, the mandible deviated towards the affected side during mouth opening, slightly roll rotation of the occlusal plane with no pain and infection. The reduction in the height of the ramus was compensated with muscular and dental adaptations. Moreover, dental extrusion caused a maximum intercuspation on the unaffected side and dental intrusion on the side affected, causing a small rotation of the occlusal plane. However, despite it, dental adaptations were mild and did not cause any noticeable aesthetic problems.
Elastic therapy was started with 2-3 Class II elastic bands and monitored twice a week. The elastic bands were gradually removed once the patient could keep a stable and reproducible occlusion that lasted for 4 weeks maximum.
The patient was called back for a follow-up after 6 to 12 months. In addition, the occlusion and mouth opening of the patient were monitored. He did not show any significant reduction in mouth opening or premature occlusal contact/open bite.
References
An Alternative Approach for Treating Severe Injured Temporomandibular Joints by Gunshot Wounds https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6933982/



