Novel coronavirus involves yet another organ causing acute pancreatitis in a 61-year-old patient. Both the virus and the medications used to manage COVID-19 patients can cause acute pancreatitis.
Approximately 17% of the severely ill COVID-19 positive patients suffer a pancreatic injury (acute pancreatitis) with elevated serological markers such as serum amylase and lipase. Another 7% of patients exhibit radiographic findings consistent with pancreatitis.
An otherwise healthy, 61-year-old male presented with fever, dyspnea, and dry cough for the past 5 days. The patient was in close contact with his father, who had been tested positive for COVID-19 (SARSCoV2).
The doctors admitted the patient to the hospital, then they performed plain chest radiography. The CXR revealed showed bilateral opacities compatible with viral pneumonia. They also ordered nasal and throat swabs for real-time transcription-polymerase chain reaction (PCR) assay.
The swab results were positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The patient developed severe pneumonia on the third day of hospital admission. The patient developed fever, weight loss, tachypnea, and hypoxemia; therefore, supplemental high-flow oxygen was given.
Pharmacological Management:
The doctors prescribed him the following medications:
- Azithromycin 500 mg OD for 3 days
- Hydroxychloroquine – LD:800 mg on day 1, then 200 mg BD for 10 days
- Zinc 50 mg BD for 5 days
- Acetaminophen PRN as needed
Later, they added:
- Tocilizumab (anti-interleukin-6 receptor antibody) 400 mg I/V 2 doses
- Dexamethasone 10 mg I/V BD for 5 days then dose-tapering
- Enoxaparin 80 mg BD for 10 days
- Lopinavir/ritonavir 200 mg/50 mg 2 tables BD for 5 days
- Pantoprazole 40 mg I/V OD
His sputum culture grew Staphylococcus aureus, so they added:
- Ciprofloxacin 400 mg I/V BD
- Clindamycin 300 mg PO QID for 7 days
(OD: once daily; BD: twice daily; QID: four times daily; I/V: intravenously; PRN: pro re nata or as needed; LD: Loading dose)
After 7 days, the patient showed substantial improvement, and he no longer required high-flow oxygen.
On the 14th day of hospital day, the patient complained of diffuse abdominal pain which was sudden in onset, and it was associated with anorexia. He had no other symptoms including vomiting, diarrhea, fever, etc.
On examination, his abdomen was soft, with mild diffuse tenderness. There were no signs of peritonitis.
Serology revealed elevated leukocytes with neutrophilia, elevated serum lipase, and serum amylase levels, but alkaline phosphatase and direct bilirubin were normal.
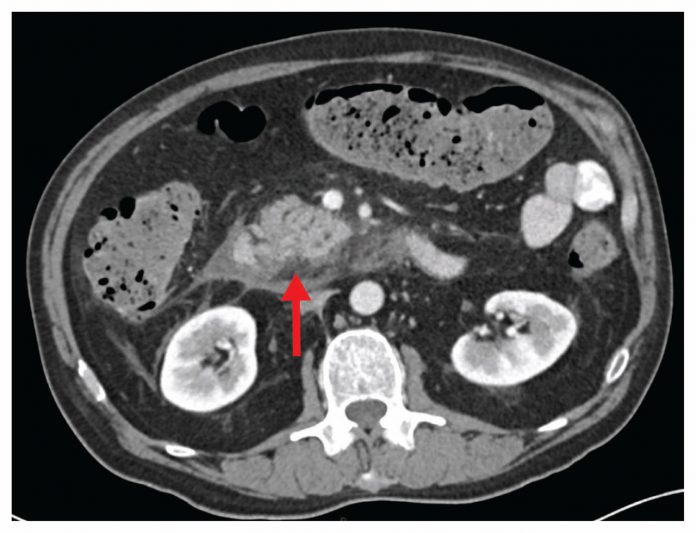
Abdominal contrast-enhanced computed tomography (CT) scan revealed signs of acute pancreatitis.
The patient received a diagnosis of acute pancreatitis.
He was started on supportive management. كيفيه لعب البوكر i.e., including nothing by mouth (NPO), intravenous fluids, and analgesics.
The patient improved within 2 days. His abdominal symptoms resolved, and liver function tests reached the baseline values. كيفية لعب القمار Further tests were performed to evaluate the etiology behind acute pancreatitis. No investigations or history clues found the culprit. Hence the suspicion of COVID-19 being the culprit behind acute pancreatitis seemed true! افضل موقع مراهنات عربي
References:
Shay Brikman, Veronika Denysova, Husam Menzal and Guy Dori, CMAJ July 27, 2020 192 (30) E858-E859; DOI: https://doi.org/10.1503/cmaj.201029
Wolfe D, Kanji S, Yazdi F, et al. Drug-induced pancreatitis: a systematic review of case reports to determine potential drug associations. PLoS One 2020; 15:e0231883
Liu F, Long X, Zhang B, et al. ACE2 expression in the pancreas may cause pancreatic damage after SARS-CoV-2 infection. Clin Gastroenterol Hepatol 2020 Apr. 22 [Epub ahead of print]. S1542–3565(20)30537–1. doi: 10.1016/j.cgh.2020.04.040



