A 37-year-old man, known case of hemophilia type A, presented to the orthopedic clinic with complaints of progressive difficulty in walking with recurrent swelling of the left thigh and progressive shortening of the leg.
The patient had a history of inadequate factor VIII replacement therapy. He also had a 10-year-old history of a traumatic left femoral shaft fracture, which was treated without surgery. The healing of the fracture was complicated by the malunion of the fracture. During these 10 years, the patient had multiple episodes of swelling of the left thigh and shortening of the leg, hampering his ability to bear weight on the left leg, so he used crutches for support during walking.
On physical examination, there was a painless swelling in the left thigh with restricted active and passive left hip movements. Also, the left leg was shorter than the right. The distance from the greater trochanter to the lateral malleolus was 10 cm shorter on the left side when compared with the right.
Serology revealed a factor VIII level of less than 1 IU per deciliter (reference range, 50 to 150).
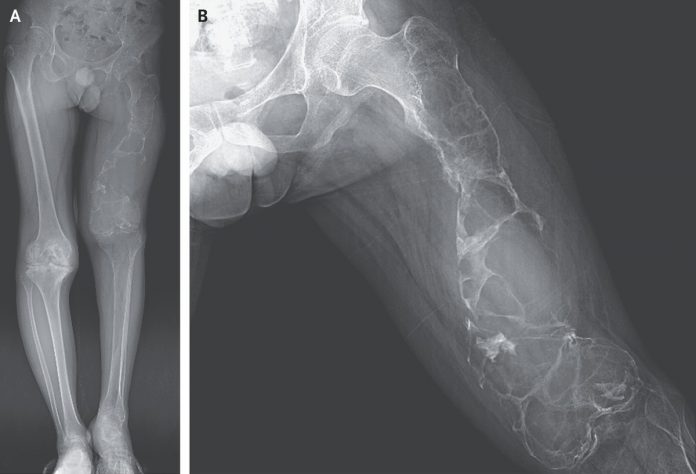
Plain Xray of the legs (Panel A), and the left femur (Panel B) in anterioposterior view showed a “soap bubble” appearance with a deformity in left femur most consistent with a hemophilic pseudotumor.
Hemophilia A is a bleeding disorder with a deficiency of factor VIII, which is one of the clotting factors playing a crucial rule in the clotting mechanism. With absent or decreased factor VIII levels, there is a bleeding tendency. Repeated bleeding episodes into the bone or soft tissues can give a rare complication of hemophilia known as the hemophilic pseudotumor.
It is quite rare and seen in 1-2% of the hemophilic patient, especially in those with severe hemophilia.
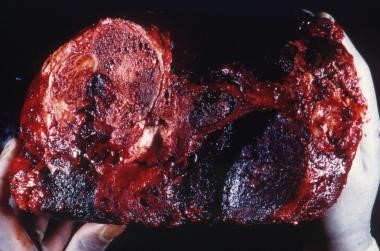
Inadequate factor VIII levels in the blood and inadequate replacement lead to recurrent bleeding into the bones, eventually forming hemophilic pseudotumor, which destroys the bone and the surrounding tissue.
Pseudotumors can either be osseous or soft-tissue lesions, depending upon the site of hemorrhages.
Clinical manifestations depend mainly on the site and severity of the hemorrhages. Symptoms may include pain, swelling, and compression of the surrounding structures. Although rare, the brownish material formed in the pseudotumor can get secondarily infected.
Plain Xray, CT scan, MRI, and even ultrasound each have a role in diagnosing and locating the pseudotumor. The management approach is primarily aimed at preserving the functional and minimizing the destruction. Depending upon the location, size, and growth rate, the management options include conservative treatment (immobilization and adequate replacement therapy), aspiration, ablation, embolization, and surgical exploration. However, surgical intervention is the most effective treatment.
References:
Zeng Li, M. a. (2020, May 21). Hemophilic Pseudotumor. Retrieved from The New England Journal of Medicine: https://www.nejm.org/doi/full/10.1056/NEJMicm1914118
Lewis TR, Webb HR, Bell JP, Beall DP, Fish JR. Hemophilic pseudotumor. J Okla State Med Assoc. 2005;98(10):485‐487.
Kamal AF, Waryudi A, Kurniawan A, Lubis AM, Gatot D. Various Surgical Treatment of Hemophilic Pseudotumor: A Case Series. Arch Bone Jt Surg. 2019;7(6):514‐522.