Night sweats, fatigue and non-productive cough in patient with rheumatoid arthritis.
This article describes the case of a 52-year-old male patient diagnosed with miliary histoplasmosis with symptoms of diarrhea, vomiting, nausea, headache, chills and fevers. The patient also reported night sweats, fatigue and a non-productive cough. His medical history revealed rheumatoid arthritis (RA), for which he was on therapy with methotrexate, weekly and hydroxychloroquine and sulfasalazine, daily. In addition, a year before he presented to the hospital, he was also taking rituximab. The medications helped manage his symptoms of RA.
The patient’s history further revealed that he was originally from Mexico, however, had been living in the US for over 40 years. Before moving to Colarado, he was living in Ohio. His occupation was of a truck driver which involved him travelling through the states of the Midwest. A month before the patient was admitted, he unloaded a truck during a rainstorm in Kansas city, after which he began having sweats and a nonproductive cough. However, he had no history of tuberculosis.
Investigation findings
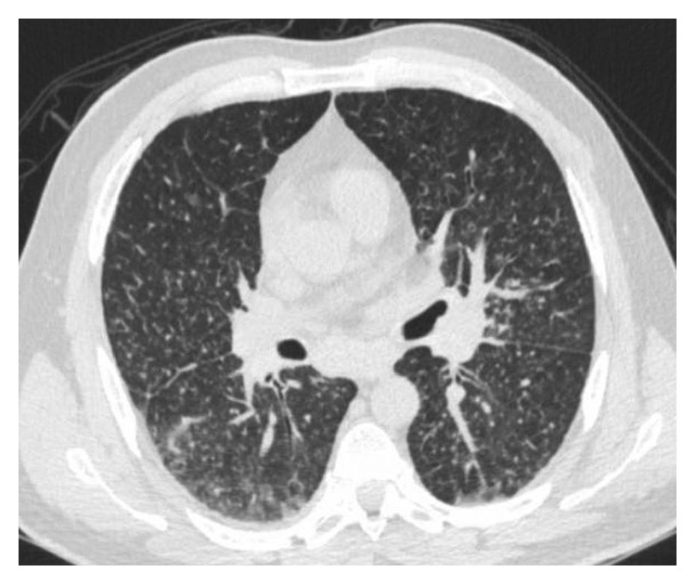
On examination, the patient had an oxygen saturation of 85%, therefore, required 2 to 3 litres of supplemental oxygen. Initial laboratory tests were significant for elevated liver enzymes. Other investigations including abdominal ultrasound showed mild hepatomegaly and the chest X-ray findings were consistent with diffuse reticulonodular density with hilar lymphadenopathy.
Doctors treated him with one dose of intravenous (IV) ceftriaxone and azithromycin. In addition, he was started on empiric treatment for pneumonia. Additional tests ruled out the possibility of an infection. However, a previous CT scan taken 6 years ago and a month ago did not show any diffuse micronodules. The findings were suggestive of a miliary pattern. Considering the patient’s clinical symptoms and history of exposure, the doctors suspected tuberculosis and invasive fungal infection. However, her AFB cultures and smear test were negative.
The patient underwent a bronchoscopy, also. The findings were notable for endobronchial plaques and nodules in the left upper lobe. All cultures came back negative so the antibiotics were stopped after 3 days. Doctors advised empiric therapy with an azole + echinocandin to cover possible fungal infection and aspergillosis. Histopathology showed necrotising granulomatous inflammation, leading to the diagnosis of an infectious aetiology. A week after treatment with liposomal amphotericin B, he was switched to oral fluconazole. The patient was discharged after resolution of hypoxia. The microbiology lab showed growth of mold from fungal lung tissue cultures nine days after discharge. A month after discharge. He was continued on oral itraconazole treatment for a year after diagnosis.
References
Miliary Histoplasmosis in a Patient with Rheumatoid Arthritis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5926488/



