A 16-year-old boy was brought to the emergency department after he fell into a 3m deep transport wagon filled with whole wheat grain. The previously healthy boy immediately submersed in the wheat grain and it took approximately 5 to 7 minutes to rescue him. When the patient was rescued, he was unresponsive, cyanotic and making spontaneous respiratory efforts.
Ventilation was a attempted using a self-inflating bag and mask when he was being transferred to a peripheral hospital via an ambulance, however, there was no obvious gas exchange because of a lack of compliance of the respiratory system. The patient arrived to the hospital 40 minutes after the accident. He was unresponsive with equal pupils that were reacting slowly to light. Examination showed that the patient’s pulse was 120 beats per minute, blood pressure 170/80 mm Hg and he was making shallow efforts at respiration at a rate of 25-30 breaths per minute. The patient’s mouth and pharynx were cleared of the large amounts of packed grain through forceps, suction and manual extraction during direct laryngoscopy. An intravenous catheter was placed and the patient was intubated with a 7.5 mm endotracheal tube (ETT).
The endotracheal tube could only be advanced just below the level of the vocal cords and did not pass further because of impacted grain in the trachea. The patient was ventilated with a self-inflating oxygen bag through the ETT. However, no effective tidal volume could be detected by auscultation or inspection. He was administered intravenous hydrocortisone 1 g and sodium bicarbonate 88 mEq. He was shifted to the university hospital by ambulance.
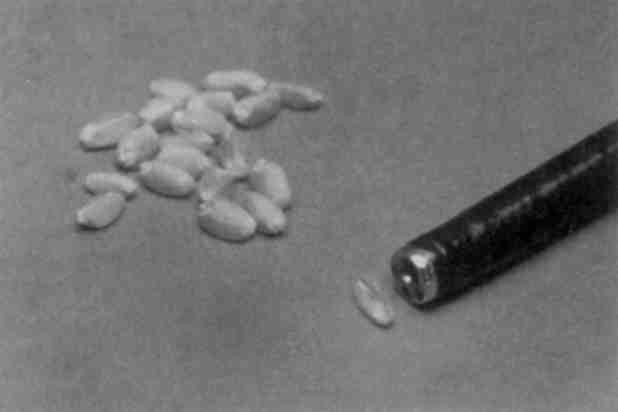
He arrived at the emergency department 2 h 4 min after the accident. The patient’s neurological status was unchanged. Blood pressure was 140/80, pulse 110 beats/min and 98% saturation by pulse oximetry. He was making shallow efforts at gasping. Bilateral emphysema was noticed in the subcutaneous emphysema. The patient was administered intravenous sodium thiopental, 300 mg, in case of subsequent hypoxemia during bronchoschopy for possible cerebral protection. The high inspiratory pressure requirement made manual ventilation difficult. Blood sample showed extreme hypercapnia and acidosis. Rigid bronchoscopy was attempted and each time 5 to 10 wheat seeds were removed using alligator grasping forceps.
The grains were eventually removed with vigorous manual inflation. In addition, manual percussion of the patient’s chest allowed more grain to be dislodged with each breath. An estimate of 200 ml of wheat grain was removed with this method and the major bronchi were cleared of grain using alligator forceps. All visible grains were removed using a fiberoptic bronchoscope with suction extraction.
The patient did not show any respiratory symptoms or residual neurologic signs at his 9-month follow-up. In addition, all pulmonary function tests were normal.
References
Management of massive grain aspiration https://pubmed.ncbi.nlm.nih.gov/9357907/



