Myositis Ossificans Following Prolonged Immobilization: An Unusual Cause of Hip Pain
Myositis ossificans (MO), also referred to as heterotopic ossification within skeletal muscle, is a benign condition characterized by the formation of mature lamellar bone in soft tissues where bone does not normally exist. Although it most commonly develops after trauma, surgery, or neurologic injury, myositis ossificans can also occur in association with prolonged immobilization and systemic illness. This case illustrates an atypical presentation of myositis ossificans in a 40-year-old woman recovering from tuberculous meningitis, highlighting the importance of maintaining a broad differential diagnosis when evaluating persistent musculoskeletal pain in immobilized patients.
The patient, a previously healthy Korean woman, had been confined to bed for several weeks during recovery from tuberculous meningitis. She presented with progressive pain in the right hip, accompanied by an externally rotated and flexed posture of the affected leg. Physical examination revealed marked discomfort with passive movement of the hip and localized tenderness in the gluteal region. These findings suggested a deep-seated musculoskeletal process rather than a superficial soft tissue injury. Importantly, there was no history of direct trauma to the hip or pelvis, which might have initially obscured consideration of myositis ossificans.
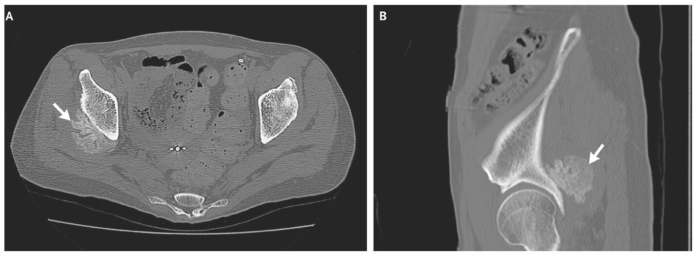
Radiographic Findings
Initial plain radiographs of the pelvis were unremarkable. This is consistent with the natural history of myositis ossificans, as early radiographic findings are often absent or nonspecific during the initial inflammatory phase. Because the patient’s pain persisted, computed tomography (CT) was performed one month later. CT imaging revealed a well-defined calcified mass within the gluteus minimus muscle, with evidence of trabecular bone formation and a surrounding cortical rim. These features are characteristic of mature myositis ossificans and help distinguish it from malignant soft tissue tumors or infectious processes.
Myositis ossificans typically progresses through three stages: an early inflammatory phase, an intermediate osteogenic phase, and a mature phase characterized by organized lamellar bone formation. During the early stage, patients often experience pain, swelling, and restricted joint movement, while imaging studies may be normal or show only soft tissue edema. As the condition evolves, peripheral mineralization becomes apparent, often described as the “zonal phenomenon,” in which mature bone forms at the periphery and less organized tissue occupies the center. This pattern is best visualized on CT and is a key diagnostic feature.
The pathogenesis of myositis ossificans is not fully understood, but it is believed to involve inappropriate differentiation of mesenchymal stem cells into osteoblasts within soft tissues. In patients with prolonged immobilization or neurologic disease, factors such as local tissue hypoxia, inflammation, microtrauma from passive movement, and altered calcium metabolism may contribute to ectopic bone formation. Neurologic conditions, including traumatic brain injury, spinal cord injury, and central nervous system infections, are well-established risk factors for heterotopic ossification, supporting the role of systemic and local inflammatory mediators.
In this patient, prolonged bed rest during recovery from tuberculous meningitis likely created a permissive environment for heterotopic bone formation. Limited mobility, sustained pressure on the gluteal muscles, and repeated passive range-of-motion exercises may have contributed to localized muscle injury and subsequent ossification. The absence of findings on early radiographs underscores the importance of advanced imaging when symptoms persist despite initial negative studies.
The differential diagnosis of a calcified intramuscular mass includes soft tissue sarcoma, osteosarcoma, calcific myonecrosis, and chronic infection. Misdiagnosis can lead to unnecessary biopsy or surgical intervention, which may exacerbate heterotopic ossification. Recognition of the characteristic imaging features of myositis ossificans is therefore critical. Biopsy is generally discouraged unless imaging findings are atypical or malignancy cannot be excluded.
Management of myositis ossificans is typically conservative. Treatment focuses on pain control, gentle physical therapy to maintain joint mobility, and avoidance of aggressive stretching or massage during the active phase. Nonsteroidal anti-inflammatory drugs (NSAIDs) may help reduce inflammation and inhibit further bone formation. Surgical excision is reserved for patients with persistent pain, functional limitation, or neurovascular compromise and is generally delayed until the lesion has fully matured to minimize recurrence.
This case emphasizes that myositis ossificans should be considered in immobilized patients with unexplained musculoskeletal pain, even in the absence of trauma. Early recognition and appropriate management can prevent unnecessary interventions and improve functional outcomes.
References
- Ackerman D, et al. Heterotopic ossification: Pathophysiology, clinical features, and the role of imaging. J Bone Joint Surg Am. 2019;101(7):650–658.
- Walczak BE, et al. Myositis ossificans. J Am Acad Orthop Surg. 2015;23(10):612–622.
- Tyler P, et al. Imaging features of myositis ossificans. AJR Am J Roentgenol. 2010;195(4):W375–W383.
- Cipriano CA, et al. Heterotopic ossification following neurologic injury. J Am Acad Orthop Surg. 2009;17(11):689–697.
- Ranganathan K, et al. Heterotopic ossification: Basic-science principles and clinical correlates. J Bone Joint Surg Am. 2015;97(13):1101–1111.