Isolated Mandibular Enlargement in an Adult Male: Atypical Presentation of Metabolic Bone Disease
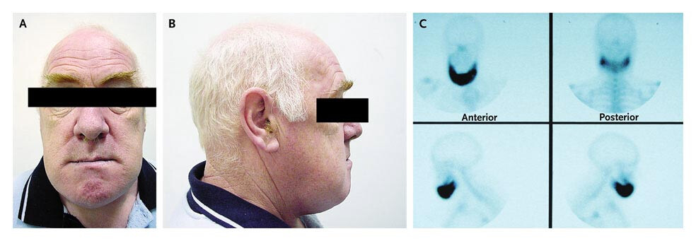
Progressive enlargement of the mandible in adults is an uncommon clinical finding that prompts a broad differential diagnosis, including endocrine disorders, neoplastic processes, and metabolic bone disease. This case describes a 55-year-old man with a two-year history of painful bilateral jaw enlargement and worsening dental malocclusion, manifested by progressively ill-fitting dentures. Notably, he lacked systemic features often associated with endocrine causes of craniofacial overgrowth, such as acromegaly, making the diagnostic evaluation particularly challenging. This article describes the case of isolated mandibular enlargement in an adult male.
On presentation, the patient denied headaches, visual-field disturbances, hyperhidrosis, oily skin, glucose intolerance, cardiomyopathy, or changes in glove or shoe size. Physical examination revealed symmetric enlargement of the entire mandible extending to the angles of the jaw, accompanied by marked misalignment of the upper and lower teeth. These findings suggested a chronic process affecting mandibular bone remodeling rather than soft tissue hypertrophy.
Laboratory Evaluation
Given the prominent jaw enlargement, acromegaly was an important consideration. Acromegaly is characterized by excessive secretion of growth hormone (GH), usually due to a pituitary adenoma, leading to elevated insulin-like growth factor 1 (IGF-1) levels and progressive skeletal overgrowth. Craniofacial changes, including mandibular prognathism, are classic features. However, in this patient, the serum IGF-1 level was normal at 15.2 nmol/L (reference range, 9–40 nmol/L), effectively excluding active acromegaly. Additionally, the absence of other hallmark clinical features further reduced the likelihood of GH excess.
In contrast, laboratory evaluation revealed elevated total serum alkaline phosphatase (ALP) and bone-specific alkaline phosphatase levels, indicating increased osteoblastic activity and accelerated bone turnover. These biochemical abnormalities strongly suggested a metabolic bone disorder rather than an endocrine growth disorder. Among such conditions, Paget disease of bone is a leading consideration, particularly in older adults presenting with localized bone pain, deformity, and increased bone turnover.
Paget disease of bone is a chronic disorder characterized by focal areas of excessive and disorganized bone remodeling. It typically affects individuals over the age of 50 and commonly involves the pelvis, spine, skull, and long bones. Craniofacial involvement, including the mandible, is well described and can lead to facial deformity, dental malocclusion, and ill-fitting dentures—features prominently observed in this patient. Bone pain is the most common symptom and is thought to result from increased vascularity, microfractures, and mechanical stress on abnormal bone.
Pathophysiology
The pathophysiology of Paget disease involves an initial phase of excessive osteoclastic bone resorption followed by a compensatory increase in osteoblastic bone formation. However, the newly formed bone is structurally disorganized and mechanically weaker. This aberrant remodeling explains both the elevated bone-specific alkaline phosphatase and the progressive bony enlargement seen clinically. Importantly, serum calcium and phosphate levels are often normal, which can delay recognition unless ALP is specifically assessed.
Radiographic imaging (not described in this vignette but typically obtained) would be expected to show characteristic features such as cortical thickening, bone expansion, and areas of mixed lytic and sclerotic change. In craniofacial Paget disease, a “cotton wool” appearance of the skull or expansion of the mandible may be evident. Bone scintigraphy is often used to assess the extent and activity of disease, as it is highly sensitive for areas of increased bone turnover.
Early recognition of Paget disease is crucial because effective treatment is available. Bisphosphonates are the mainstay of therapy and work by inhibiting osteoclast-mediated bone resorption, thereby reducing bone turnover and alleviating pain. Nitrogen-containing bisphosphonates, such as zoledronic acid, have been shown to induce long-lasting biochemical remission and improve symptoms. Treatment can also prevent disease-related complications, including pathological fractures, osteoarthritis of adjacent joints, hearing loss (with skull involvement), and, rarely, malignant transformation to osteosarcoma.
This case highlights the importance of considering metabolic bone disease in patients with isolated craniofacial enlargement and normal endocrine studies. Reliance solely on classic systemic features may delay diagnosis. Measurement of alkaline phosphatase, particularly bone-specific isoforms, plays a key role in identifying disorders of high bone turnover. A multidisciplinary approach involving internal medicine, endocrinology, radiology, and dentistry is often required for optimal diagnosis and management.
References
- Ralston SH, et al. Diagnosis and management of Paget’s disease of bone in adults: A clinical guideline. J Bone Miner Res. 2019;34(4):579–604.
- Singer FR, et al. Paget’s disease of bone: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(12):4408–4422.
- Whyte MP. Paget disease of bone. N Engl J Med. 2006;355(6):593–600.
- Seton M. Paget disease of bone: Diagnosis and drug therapy. Cleve Clin J Med. 2013;80(7):452–462.
- Corral-Gudino L, et al. Epidemiology, clinical characteristics, and management of Paget’s disease of bone. Lancet. 2017;389(10087):190–200.