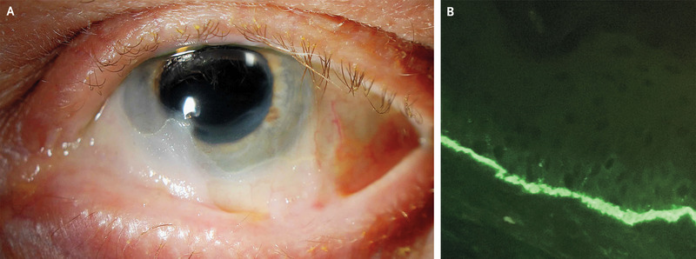
Case of Symblepharon
This article describes the case of a 73-year-old man with a history of linear IgA bullous dermatosis, diagnosed with symblepharon. Linear IgA disease (LAD) is an autoimmune subepidermal bullous disorder that may impact the skin or mucous membranes.
The 73-year-old patient presented to the ophthalmology clinic with complaints of blurry vision, photophobia and burning in both eyes with a history of 5 months. The patient also reported that he had developed lesions on his neck and scalp over this time period. His history revealed that he had not taken any new medications, nor had he recently been prescribed any antibiotics. Physical examination showed scattered vesicles and bullae on the neck, scalp, arms and back. The patient’s visual acuity was 20/30 in the right eye, whereas, 20/70 in the left eye.
Other findings included film-like adhesions between the bulbar and palpebral conjunctivae in both eyes. Based on these findings, doctors diagnosed the patient with symblepharon. Biopsy of the lesion with direct immunofluorescenceshowed a linear band indicating the presence of IgA antibodies to antigens in the basement membrane. The patient was diagnosed with IgA bullous dermatosis with ocular involvement.
Treatment
Doctors initiated treatment with dapsone and systemic topical glucocorticoids, eye lubricants and topical cyclosporin. The patient did not return for any follow-ups. Patients with an autoimmune blistering disease should also be evaluated for ocular involvement. Autoimmune blistering disorders are a group of rare skin diseases which occur when your immune system attacks the skin and mucous membranes lining the inside of the mouth, nose and other parts of the body. Whereas linear IgA may occur as a complication of various occlusal diseases, for example, as a complication of chemical burn, pemphigus bullosa, erythema multiforme, chemical injury, cicatrical pemphigoid, Steven-Johnson syndrome and dry eye syndrome. Any conjunctival infections that are complicated with conjunctival scarring may lead to symblepharon, as with this case.
Source: NEJM



