Case Report
Schwannomas are slow-growing, benign, encapsulated tumors that can arise from any neuron with a Schwann cell sheath. Stout invented the term “schwannoma” in 1935. These tumors are sometimes known as neurilemomas or neurinomas. They frequently appear as gradual, painless lumps in the head and neck, accounting for 25-45% of cases. Schwannomas prefer places such as the parapharyngeal space, lateral neck, and temporal bone, and they can develop at any age. These are typically encapsulated, with the exception of those from the sinonasal tract and nasopharynx.
Case Presentation
The current case involved a 38-year-old female Indian patient who had been complaining of headaches, facial heaviness, and loss of smell for the previous two years. Previous medical and familial history had no bearing on the outcome. She completed many courses of antibiotics and anti-inflammatory medicines by her doctor for chronic rhinosinusitis, but the symptoms did not improve. She was diagnosed with chronic rhinosinusitis and had functional endoscopic sinus surgery.
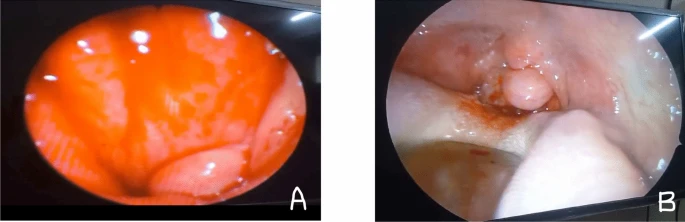
During the surgery, a solitary smooth swelling was emerging from the posterior wall of the nasopharynx, as illustrated in Fig. 1. The lump was covered with normal-looking mucosa that did not cross the midline. Furthermore, the tumor seemed to be a well-encapsulated, pink, firm, and fairly vascular mass that extended into the oropharynx without bulging over the soft palate. An examination of the ear, oral cavity, and neck revealed no notable findings. A cranial nerve evaluation indicated no further sensory or motor abnormalities.
Investigation:
In terms of radiology, contrast-enhanced computed tomography (CECT) of the neck revealed a well-defined polypoid soft tissue attenuation lesion originating from the nasopharynx’s posterior and left lateral walls and extending into the lumen. Post-contrast computed tomography (CT) demonstrates uniform contrast enhancement. No visible expansion beyond the nasopharynx was observed.
The tumor was removed en bloc using an endoscopic combination transnasal/transoral technique under general anesthesia, . The tumor originated at the junction of the posterior and lateral walls of the nasopharynx, slightly below the inferior margin of the torus tubarius on the left side. However, the patient’s post-operative recuperation was unremarkable.
The mass was submitted for histology and immunohistochemistry (IHC).
Histopathological examination revealed a well-defined, unencapsulated lesion beneath the pharyngeal mucosa. The lesion had slender spindle cells with a varied distribution pattern. The cellularity of the lesion was primarily homogeneous, with nuclear palisading in localized places. No atypia or enhanced mitosis were seen. No areas of coagulative necrosis or high-grade transformation were seen.
Immunohistochemistry reveals a benign nerve sheath tumor resembling schwannoma, with tumor cells positive for S100 (immunoreactive; score in lesional cells) and SOX10. CD34 is not immunoreactive, however KI67 is immunoreactive in 2-3% of lesional cells, confirming neurological origin. The histological characteristics are suggestive of cellular schwannomas.
The patient showed no evidence of recurrence after 6 months of observation.
Discussion
Schwannomas and neurofibromas are neurogenic tumors that arise from Schwann cells. Neurofibromas develop from the perineurium, which is inseparable from the nerve of origin. Schwannomas, on the other hand, can be surgically excised from their nerve of origin due to the preservation of the nerve’s functional and morphological integrity along its longitudinal growth axis, giving the tumor a distinct fusiform look. This anatomical differential enables for the microscopical separation of schwannomas and neurofibromas.
These schwannomas are often well-defined and well-encapsulated masses that are frequently asymptomatic and grow slowly, at a pace of 2.5-3 mm each year. Schwannomas can be difficult to diagnose because to their nonspecific and occasionally misleading presentation. On plain CT scans, schwannomas normally seem hypodense compared to muscle. On contrast CT these lesions typically demonstrate some degree of peripheral enhancement.
In this case, the patient had been experiencing a foreign body sensation in his throat for the previous 6 months as a result of a Schwannoma in the nasopharynx. Because the lesion is thought to have a vascular origin, a biopsy is usually a relative contraindication for parapharyngeal malignancies. As a result, we did not undertake a pre-operative biopsy in this case. The fundamental goal of therapy is to safeguard the neurological structures connected with the tumor while completely removing the tumor itself. The prognosis following surgery is usually positive, while recurrences can occur on occasion.