Case report
Nicolau Syndrome (NS) is an uncommon yet clinically significant illness. This condition, also known as embolia cutis medicamentosa, Nicolau livedoid dermatitis, and livedo-like dermatitides, is a severe vascular complication associated with numerous routes of medication administration, most commonly intramuscular injections. This condition begins with localized vasospasm reflex-induced discomfort and pallor, followed by erythema, livedoid or hemorrhagic lesions, and blisters. It eventually leads to a variety of necrotic symptoms.
Nicolau syndrome is generally diagnosed through a clinical history and examination. This syndrome is associated with a number of serious consequences, most notably regional skin necrosis at the injection site. That can lead to ulceration and scarring. There is a higher risk of subsequent infections such cellulitis or abscess formation. Patients frequently experience significant pain, and in severe cases, massive tissue loss may necessitate surgery or skin grafting treatments. Obviously, skin changes can have a major impact on the patient’s psychological life and self-confidence. This is more crucial to care for in the pediatric population.
The clinical relevance of NS is due to its varied presentation. It can range from minor symptoms to severe and potentially fatal results, largely defined by necrosis of subcutaneous adipose tissue and underlying musculature. As a result, quick detection and therapeutic action are important to avoiding catastrophic problems. A case of a 4-year-old child, who was diagnosed with NS following an intramuscular triamcinolone acetonide injection. And received comprehensive treatment with preventive antibiotics, analgesics, and antithrombotic medication.
Case presentation
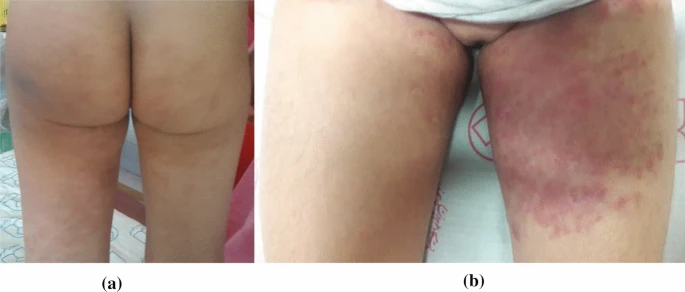
A 4-year-old Iranian girl was brought with significant swelling and discolouration in her buttocks, as well as extreme pain that made it difficult to walk. The symptoms developed following a 20 mg intramuscular injection of triamcinolone acetonide. That was administered to treat the patient’s developing vitiligo. Notably, within 30 minutes post-injection, the patient displayed discolouration at the injection site. That later extended to include the upper and lower left leg over several hours.
Clinical examination indicated ecchymosis and a cyanotic patch at the injection site, along with the formation of a livedoid look. Physical examination revealed warmth, induration, and significant discomfort around the injection site. The patient’s family history did not include any dermatological, thrombotic, or autoimmune illnesses. The girl had no severe comorbidities other than vitiligo, for which she was being treated with topical corticosteroids and pimecrolimus cream. There were no reported allergies.
Aside from thrombocytosis (platelet count: 450,000) and high D-dimer levels, laboratory tests revealed no notable findings. The patient had imaging examinations, and the ultrasound imaging revealed substantial swelling and inflammation but no indication of abscess formation, allowing us to rule out infectious differentials such as cellulitis.
The patient’s clinical presentation, medical history, and imaging data were used to make a conclusive diagnosis of NS.
Management
Immediate treatment included the injection of enoxaparin (1.5 mg/kg/dose twice daily), warm compresses, prophylactic antibiotics, and acetaminophen for pain relief. Enoxaparin was continued for ten days, and other supporting measures were maintained for one week. Symptom progression stopped within one day of starting medication, with skin symptoms improving over two weeks and inflammatory and subcutaneous edema clearing up over four weeks. The patient’s parents were pleased with the treatment outcome, and there were no side occurrences. This case demonstrates the potential problems of intramuscular corticosteroid injections in young patients, highlighting the importance of early detection and care of NS to prevent further morbidity.
Discussion
A 4-year-old girl developed signs of NS after having a corticosteroid injection.
NS is a rare but clinically severe complication that can occur after any type of medication injection. Although this consequence is more common with intramuscular injections, it has also been reported after subcutaneous and intra-articular doses. NSAIDs, antibiotics, corticosteroids, antipsychotics, antiepileptics, vaccinations, antihistamines, local anesthetics, and even other substances such as interferon alpha, cyanocobalamin, bismuth, vitamin K, and vitamin B complex have all been linked to this syndrome.
NS is distinguished by painful edema in the afflicted area quickly after the injection, which is frequently accompanied by prominent purplish staining of the skin. This initial presentation may indicate vascular impairment and an inflammatory reaction, and it can escalate to more serious symptoms. The subsequent development of livedoid erythema and isolated hemorrhagic patches is indicative of the continued vascular phenomena and tissue injury.
As the illness progresses, severe necrosis can develop, affecting not just the dermal and subcutaneous layers, but also the underlying muscle tissue. This highlights the need of quick detection and action. Early detection and effective therapy measures are critical to prevent substantial tissue damage and improve patient outcomes in cases where NS is suspected.
In the majority of recorded cases, the symptoms began with acute pain immediately following the injection; however, this was not true for all individuals. Stoehr and colleagues described a case involving a 38-year-old male who had a corticosteroid combination injection. Symptoms included numbness in the left leg 6 hours after injection, followed by pain 12 hours later. In another instance reported by Ruffieus and colleagues, a 79-year-old man who received a corticosteroid combination injection was hospitalized 2 days after the injection due to decompensated diabetes, and a livedoid lesion was found on the right buttock during the course of hospitalization.