Case Report
Neurobrucellosis (NB) is a condition caused by the bacteria Brucella. It can cause a variety of health concerns, making diagnosis difficult. The brain and nerve system can be affected for a long period, and symptoms may be mistaken as tuberculosis. Brucellosis is a frequent disease in the Mediterranean and Middle Eastern regions, resulting in around 500,000 new cases reported globally each year.
The principal mode of transmission is to consume unpasteurized dairy products, such as fresh milk and cheese. Infection can also result via eating undercooked meat, coming into contact with infected animals, or inhaling the germs. This disease may have effects on the nervous system, with a prevalence of 3–10% of cases. Although neurobrucellosis is infrequent worldwide, it is more common in areas with a greater brucellosis prevalence. And it accounts for only 0.5% of all brain and spinal cord infections. This condition can significantly affect the brain and spinal cord, resulting in infections and nerve-related issues.
This can cause inflammation, strokes, and, in rare situations, psychological issues. Brucellosis is a systemic condition that causes neurological symptoms such severe headaches, disorientation, depression, and behavioral disturbances. Other symptoms may include fever, weariness, muscle and joint discomfort, anorexia, malaise, and perspiration. In some situations, it can result in orchitis, endocarditis, and hepatosplenomegaly. The onset of symptoms might be quick in a few days or occur chronically, making it a possible diagnosis in chronic instances.
Neurobrucellosis
The prevalence of atypical symptoms may make neurobrucellosis challenging to diagnose. However, particular abnormalities on a brain scan can help determine the diagnosis. Even if you have never consumed unpasteurized milk before, you should be extremely cautious. Culture is the most effective approach, however it may have low sensitivity, particularly in NB. When cultures are negative, serological tests are critical in determining the diagnosis. Despite the widespread incidence of Brucella infection and the known risk of meningitis as a consequence, there have been few documented cases of neurobrucellosis, which encompasses meningitis, myelitis, and radiculoneuritis.
This shows that Brucella meningitis situations may be underreported due to their resemblance to tuberculous meningitis, which is common in areas where diagnostic problems exist. When examining patients, physicians should evaluate the possibility of brucellosis. As a result, clinical suspicion is critical for quick diagnosis and treatment, preventing serious sequelae. In human brucellosis, a combination of two or more antibiotics has been shown to be highly successful, with minimal recurrence rates. Furthermore, the combination of ciprofloxacin, doxycycline, and rifampicin was shown to be more effective in treating neurobrucellosis. This instance of Brucella meningitis presented as persistent, intractable headache, highlighting the possibility of Brucella meningitis as a cause of chronic headache, particularly in endemic locations.
Case Presentation
A 25-year-old unmarried Syrian girl arrived at the hospital with a developing frontal headache that had increased after lying down for a month and no other symptoms. The patient had no medical history, no previous medication use, no surgical history, and no family history. Classic tests and investigations, such as full blood counts, returned normal results. It was diagnosed as a frontal headache and treated with medications.
After two weeks, she returned to the hospital since her symptoms had not improved. She continued to have the same headache that woke her up, along with photophobia, impaired vision, tinnitus, nausea, and vomiting. There were no further systemic symptoms or fever present. She was admitted to the hospital, and her medicine was discontinued.
Examination
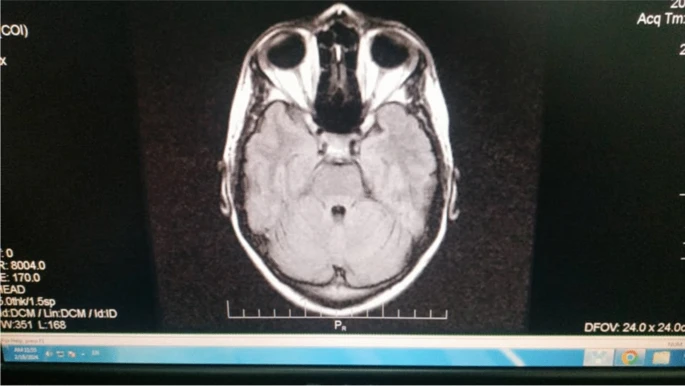
The patient had all essential neurological examinations, and the clinical examination revealed grade 2 papilledema. The remainder of the exam was negative, including meningeal symptoms. The laboratory tests were all normal. The cerebral magnetic resonance imaging (MRI) was normal, as illustrated in Figure 1. Then, 5 days after admission to the hospital, cerebrospinal fluid (CSF) aspiration was performed, yielding 20 white blood cells and 86,000 red blood cells. The sugar and protein levels in the CSF were within normal limits, however the opening pressure was discovered to be increased. As a result, she was diagnosed with idiopathic intracranial hypertension and was prescribed acetazolamide. The patient was discharged.
Over a 10-month period, the patient experienced a persistent headache without any other symptoms, leading to multiple treatments with amitriptyline and painkillers.
After several months, the patient returned complaining of a persistent headache accompanied by bilateral diplopia and esotropia, prompting admission to the hospital for 5 days. She did not describe any systemic symptoms. Upon clinical examination, the patient had bilateral sixth nerve palsy with no other meningeal symptoms or fever, as well as bewilderment. In addition, there was grade 3 bilateral optic disc edema. The remainder of the physical evaluation was normal.
Investigations
Several tests were performed, including a chest X-ray (normal), an MRI, and brain magnetic resonance venography (MRV) (also normal). CSF analysis revealed an elevated opening pressure, a white blood cell count of 40 mm3/cells, 1000 red blood cells, elevated protein at 85 mg/dL, lower CSF glucose at 42 mg/dL, and blood glucose at 110 mg/dL. The CSF culture was negative, the PCR for tuberculosis (TB) was negative, the erythrocyte sedimentation rate (ESR) was 12 mm, and the Wright’s reaction was 1/160. Brucella antibodies were found in both blood and CSF samples, despite the lack of classic brucellosis symptoms such as fever or joint inflammation.
Consequently, the patient was diagnosed with Brucella meningitis. The patient was given rifampicin, doxycycline, and ceftriaxone for 8 weeks. The patient began to improve during a follow-up visit, four weeks after starting treatment. Upon examination, bilateral diplopia and esotropia faded, and the headache began to subside.