Case Report
Kartagener syndrome (KS) is a subset of the larger category of ciliary motility disorders known as primary ciliary dyskinesias (PCDs).
Chronic sinusitis, bronchiectasis, and situs inversus make up the clinical triad of the illness. In KS, mutations in the dynein axonemal intermediate chain 1 (DNAI1). And dynein axonemal heavy chain 5 (DNAH5) genes reduce ciliary motility. Thereby, increasing the risk of infertility, left-right body alignment issues, and recurrent sinopulmonary infections. Normal ciliary activity is vital for sperm motility, respiratory system defense, and appropriate alignment of internal organs during development.
During the embryonic phase, constant ciliary movement determines the placement of internal organs. However, in Kartagener syndrome (KS), the organs do not migrate to the left side due to decreased ciliary movement, resulting in situs inversus. Individuals with KS frequently develop recurrent respiratory infections due to inadequate mucociliary clearance. There is no gold standard diagnostic test for PCD, hence it requires numerous complimentary tests. The European Respiratory Society recommends nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing.
If TEM is not accessible, immunofluorescence labeling of ciliary proteins can provide a reliable diagnosis. Overall, ciliary ultrastructure and beat pattern correspond well with genotype. Nevertheless, 26% of reported PCD patients (by genetics, nNO, and TEM) lack ultrastructural abnormalities. It affects females and males are equally. The worldwide incidence of PCD ranges from 1 in 20,000 to 1 in 40,000 births. KS occurs in around one in every 32,000 births worldwide. The frequency or incidence of Kartagener syndrome (KS) in Ethiopia is unknown. And there are only a few case reports, underscoring the condition’s rarity. Factors such as being a low-middle-income country, which limits access to diagnostic testing, may contribute to the disease’s infrequent identification.
This report details the case of a 17-year-old kid diagnosed with Kartagener syndrome. This case report seeks to positively influence the scientific community by emphasizing the necessity of early detection and intervention in this disease.
Case Presentation:
A 17-year-old Black African Semitic male patient visited our hospital with an intermittent cough that produced thick, yellowish mucous. When he was five years old, he had a cough but did not seek medical assistance. His first visit to a healthcare facility was five years ago, when he complained of nasal congestion, sneezing, and difficulties smelling. He sought treatment at several hospitals and was checked by an ENT specialist, who diagnosed him with chronic sinusitis. He was given saline rinses and augmentin 625 mg three times a day. After this, his symptoms improved for a few weeks.
He had received multiple treatments for lower respiratory tract infections at local health facilities. He used to experience an intensification of these symptoms every 2-4 weeks. And he is currently suffering from a progressive deterioration of his productive cough, which is worse by walking for more than 30 minutes. And reduced by taking frequent breaks. He also has a history of nasal congestion and recurrent sneezing. He sought treatment at a local health center before being referred to our hospital. However, he has no history of smoking or alcohol consumption. His mother said that he was born at home following a full-term pregnancy through spontaneous vaginal birth. He has no substantial developmental deficits. He is the firstborn kid and has one younger brother; no other family members have reported similar concerns.
Examination
On physical examination, he was quite stable, with normal vital signs. His blood pressure was 120/80 mmHg, with a pulse rate of 88 beats per minute and a respiratory rate of 24 breathes per minute and oxygen saturation was 94% on room air.
There were no visible nasal polyps, no signs of chest deformity or nasal flaring, no subcostal or intercostal retractions, coarse crackles in the left posterior lower lung field, no cyanosis or clubbing, normal heart sounds at the base of the heart on the right side, and the point of maximal impulse was located at the right fifth intercostal space. There were no murmurs or gallops.
Investigations:
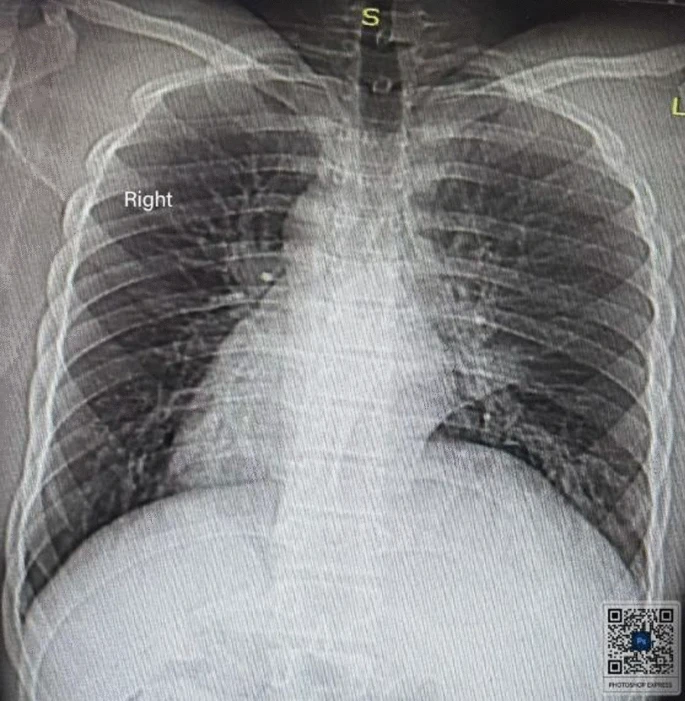
He was admitted to the medical ward for examination. A chest X-ray in the posterior-anterior (PA) view showed dextrocardia, a gastric shadow on the right side, and bronchiectatic alterations near the left cardiac boundary. A high-resolution chest computed tomography (CT) scan revealed the complete reversal of the heart and main arteries, demonstrating dextrocardia. The abdominal organs visible on the CT scan included the stomach and spleen on the right and the liver on the left, showing complete situs inversus. In addition, the left lower lobe showed bronchiectatic alterations.
An electrocardiogram (ECG) indicated a right axis deviation, an inverted P wave in lead I, and an avL, indicating dextrocardia. A two-dimensional echocardiography showed dextrocardia, with all four chambers normal. A Doppler examination confirmed a dextrocardia with situs inversus of the aorta and inferior vena cava. Routine laboratory testing to rule out simultaneous infectious processes, such as the total blood count and erythrocyte sedimentation rate (ESR), came back normal. The liver and kidney function tests, as well as fasting blood sugar levels, were all within acceptable limits.
Following a thorough review and imaging studies, he was diagnosed with Kartagener syndrome. He spent three days in the hospital. He received education and counseling on his condition. Upon discharge, he was advised to undertake thoracic physiotherapy, take azithromycin 500 mg three times per week, and guaifenesin syrup 200 mg three times per day. Thoracic physiotherapy for Kartagener syndrome focuses on using techniques such as postural drainage, percussion, and vibrations to aid in mucus clearance from the airways, as the condition causes compromised ciliary function, making it difficult for the body to expel secretions naturally.
Followup
After a month, the patient reported improved cough and exacerbation three weeks after discharge. He sought help at a health center and was treated with cephalexin, resulting in significant improvement after four days. Vital signs were normal, but he had coarse crackles in the left lower lung.
The patient continued his azithromycin and chest physiotherapy regimen, reporting no exacerbations and increased exercise tolerance. He was recommended to continue chest physiotherapy, take azithromycin three times weekly, and receive vaccinations for influenza and pneumococcal disease.