Case Presentation
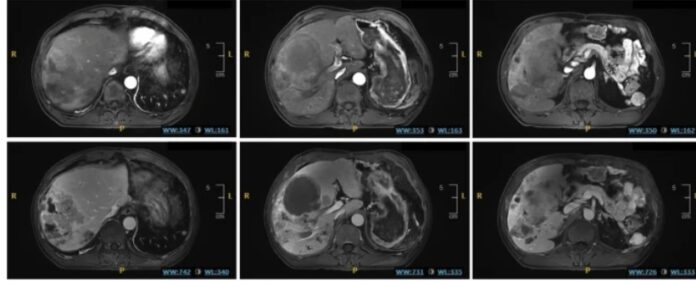
A 52-year-old male patient with advanced Hepatocellular carcinoma developed Tumor lysis syndrome (TLS) after receiving Hepatic artery infusion chemotherapy (HAIC). The patient presented with multiple liver tumors and lung metastases. In addition, the doctors had administered two prior cycles of HAIC with some initial clinical benefit. During the third cycle of HAIC, he experienced a rapid deterioration in his condition. This was characterized by severe abdominal pain and a significant decline in kidney function.
The patient’s clinical presentation, including fever, abdominal pain, decreased urine output, and elevated levels of potassium, phosphorus, and uric acid in the blood, strongly suggests the development of TLS. Furthermore, he experienced seizures, a serious neurological complication often associated with TLS.
The medical team promptly initiated aggressive management strategies to address the TLS. These strategies included intravenous fluid administration to enhance renal perfusion and prevent dehydration. Doctors implemented pharmacologic interventions to lower uric acid levels, correct electrolyte imbalances, and protect the kidneys. Additionally, they employed renal replacement therapy in the form of dialysis. They did this to temporarily assist the kidneys in removing waste products from the bloodstream. Despite the severity of the situation, the patient responded favorably to the intensive treatment regimen. He was eventually discharged from the hospital.
Introduction to Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC), a primary liver cancer, presents a significant global health challenge. Characterized by its insidious onset and often aggressive progression, HCC frequently presents at an advanced stage. It significantly impacts patient prognosis. Advanced HCC is typically defined by the presence of large tumors, the spread of cancer within the liver, or the presence of metastases to other organs, such as the lungs or bones. In these advanced stages, treatment options become more limited, and achieving durable disease control becomes a significant challenge.
Management of Hepatocellular Carcinoma
Hepatic artery infusion chemotherapy (HAIC) has emerged as a promising therapeutic approach for advanced HCC. Unlike systemic chemotherapy, which is administered intravenously and circulates throughout the entire body, HAIC delivers chemotherapy directly to the liver through the hepatic artery. This is the major blood vessel supplying the liver. This targeted delivery approach concentrates the chemotherapeutic agents within the liver. It maximizes their impact on the tumor while minimizing systemic exposure and associated side effects.
Studies have demonstrated that HAIC can offer superior survival outcomes compared to systemic chemotherapy or other standard treatments, such as sorafenib, particularly in patients with extensive liver involvement. This enhanced efficacy is attributed to the concentrated delivery of chemotherapy. This allows higher doses to reach the tumor while limiting systemic exposure and associated side effects. This localized delivery not only increases the effectiveness of the chemotherapy but also reduces the potential for side effects that can occur when chemotherapy circulates throughout the entire body.
Tumor Lysis Syndrome
However, as with any potent therapy, the use of HAIC can be associated with potential complications. Tumor lysis syndrome (TLS) is a serious, albeit rare, complication that can arise during cancer treatment. TLS occurs when a significant number of cancer cells die rapidly, releasing a surge of intracellular components, such as potassium, phosphorus, and uric acid, into the bloodstream. This sudden influx of these substances can overwhelm the body’s regulatory mechanisms, leading to a cascade of metabolic disturbances.
TLS is more commonly observed in hematologic malignancies, such as leukemia and lymphoma. However, it can also occur in patients with solid tumors, including HCC, although with a lower frequency. While TLS has been reported in association with other HCC treatments, such as transcatheter arterial chemoembolization (TACE) and targeted therapies like Sorafenib and Lenvatinib, cases specifically linked to HAIC are relatively rare.
Discussion
This case serves as a potent reminder that even with effective therapies like HAIC, serious complications can arise. Vigilant monitoring of patients during and after treatment is crucial to promptly identify and manage potential adverse events. While the incidence of TLS in the context of HAIC for HCC may be low, its potential for severe consequences highlights the importance of heightened clinical awareness and a proactive approach to its management.
There is a need for a high index of suspicion for TLS in patients with HCC undergoing aggressive therapies, particularly those with a high tumor burden or those who demonstrate a rapid response to treatment. Early recognition and immediate implementation of appropriate treatment strategies are essential for optimizing patient outcomes and minimizing the potential morbidity and mortality associated with this life-threatening complication.