Case report
Hao-Fountain syndrome (HAFOUS) is a rare neurodevelopmental disorder with a global prevalence of 1/1,000,000. Fountain et al. originally defined it in 2015, when they reported six children with various neurodevelopmental problems. Global developmental delay, variably impaired intellectual development with significant speech delay, behavioral abnormalities along with mild dysmorphic faces were among the first clinical features.
Fountain et al. published a detailed article in 2019 that described the behavioral and physical characteristics of 16 patients, including prominent speech delays, intellectual disability ranging from borderline intellectual functioning to mild-moderate intellectual disability. And autism spectrum disorder (ASD) diagnosis or autistic features in some children. In addition, patients also found to have impulsivity, compulsivity, stubbornness, manipulative behaviors, a proclivity for temper tantrums and violent conduct along with attention deficit hyperactivity disorder (ADHD)
Physical Characteristics
Physical characteristics include facial dysmorphisms, hypogonadism, altered pain thresholds, gastroesophageal reflux disease (GERD). A history of eating issues, seizures, and abnormal brain magnetic resonance imaging (MRI) results. Difficulties in coordination tests and managing a sequence of motions and decreased pain sensitivity.
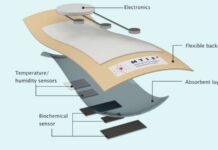
A rare condition that affects multiple body functions and structures requires a multidisciplinary team management. That includes physicians, occupational therapists, speech pathologists, physiotherapists, psychologists, social workers, administrative staff, specialist medical services, and allied health providers. The purpose of this report is to shed light on the syndrome’s impact on patients’ daily living functions and caregivers. As well as the importance of a multidisciplinary treatment approach.
Case Presentation
The patient is a 5-year-old Persian girl, the second child of consanguineous and healthy parents. She was identified with Hao-Fountain syndrome using whole-exome sequencing. She was born at 38 weeks of pregnancy, weighing 3100 g, with a height of 51 cm. And a head circumference of 37 cm, and her growth metrics at the time of the report were 120 cm, 25 kg, and 52 cm. The anomaly scan showed an echogenic itra cardiac focus thrice. Her hypotonia and trouble nursing were obvious from birth. She spent 5 days in the neonatal intensive care unit (NICU) due to low blood sugar and patent ductus arteriosus.
At two months old, she was diagnosed with vesicoureteral reflux (VUR) due to frequent urine infections. The kidney had normal size, shape, and echotexture. While the distal region of the uterus was moderately dilated. Bilateral high-grade vesicoureteral reflux was identified using a catheter-based technetium-99m pretechnetate scan of the bladder. At the age of six months, she had a gel injection (hyaluronic acid/dextranome) into the bladder wall for VUR treatment. But it was unsuccessful, therefore she had surgery (ureteroocystostomy) at two years old.
Some facial dysmorphisms akin to Down syndrome and hypotonia prompted the medical team to rule out this diagnosis using karyotyping. According to the International System for Human Cytogenomic Nomenclature (ISCN, 2016), the patient’s karyotype was 46, XX (normal female). she underwent whole-exome sequencing (WES) based on her phenotype, resulting in the detection of a potentially pathogenic variation in the ubiquitin-specific peptidase 7 (USP7) gene at 2.5 years of age. Sanger sequencing confirmed that the mutation was heterozygous in our patient, but her parents and older brother were normal.
The USP7 gene’s deubiquitinating activity regulates many target proteins and interactors. And it plays an important role in regulating the stability of proteins involved in critical cellular processes.
Investigation
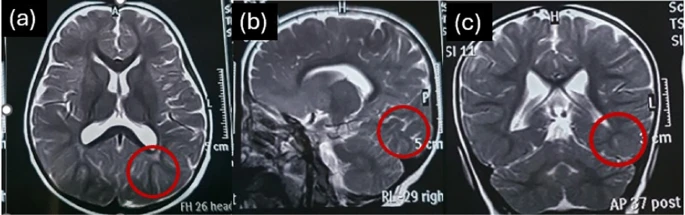
At the age of two years, the brain MRI report revealed modest dilation of occipital lobe sulci. And mildly elevated signals in the white matter next to the lateral ventricle’s trigone. When she was one year old, electroencephalogram (EEG) data revealed dysrhythmic discharges in both hemispheres, prompting a pediatric neurologist to prescribe pirimidon. The MRI report at the age of two years was normal although slightly hazy. EEGs performed twice a year to track aberrant discharges over time that showed frequent generalized epileptic discharges (spike). At the ages of three and four, she experienced two generalized tonic colonic seizures. As well as some focal seizures, and she was kept on sodium valproate and diazepam. After two years of medicinal therapy, epileptic discharges appear to be under control.
Her sleep difficulty has been persistent for about two years, but her sleep patterns have just returned to normal. Recurrent respiratory infections have always resulted in increased antibiotic use. The main clinical symptoms of this syndrome are hypotonia, delays in milestone attainment, speech delays, substantial behavioral abnormalities such as refusal to follow rules. And poor gross motor control and ataxic gait, according to occupational therapy and speech pathology examinations. She said her first word when she was three years old and continued to speak in single words for about six months.
Walking milestones were completed after 6 months of regular neurodevelopmental occupational treatment at the age of two years. Dynamic balancing is a challenge for her. Postural issues such as back knee deformity and forefoot pronation are also evident, resulting in imbalance while standing or walking.
She was not formally evaluated using a standardized intelligence quotient (IQ) test, but special schooling is required for age-related learning. She had never been formally diagnosed with autistic spectrum disorder (ASD), although she did show symptoms like poor eye contact. Hyperactivity and difficulty attending age-appropriate play and activities have long been a source of family concern.