A patient with a childhood history of easily-bleeding, painful blue nodules gets a diagnosis of blue rubber bleb nevus syndrome (BRBNS).
A 31-year-old man presented to the outpatient department of dermatology with complaints of painful blue nodules since forever. The patient reported a diffuse distribution of the nodules throughout the body. Moreover, he revealed that the lesions bled easily.
Family history revealed similar lesions in his uncle and father.
Earlier, the patient had consulted other physicians, and they had performed a biopsy of the lesions, but they could not reach a conclusive diagnosis.
Past medical history did not reveal any complaints of epistaxis (bleeding from nose), hematemesis (blood in vomitus), haematuria (blood in urine) or blood in his stool. However, history showed evidence of iron deficiency anaemia.
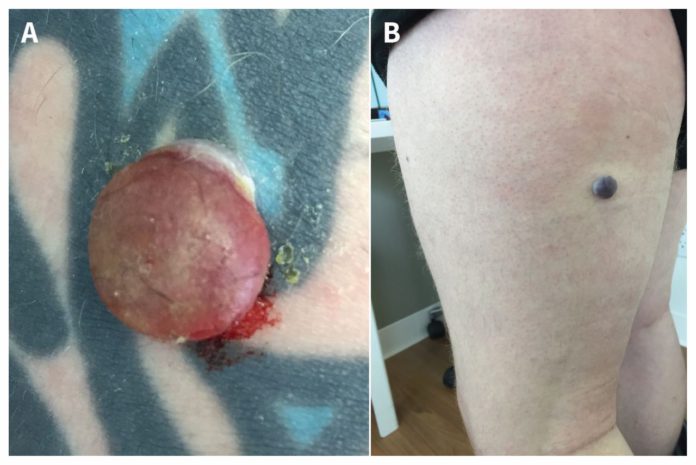
Physical examination revealed approximately 20 blue nodules. These nodules were distributed throughout the upper and lower extremities, abdomen and buttocks.
Owing to his clinical presentation, dermatologists suspected blue rubber bleb nevus syndrome (BRBNS). It is a rare disease with less than 200 reported cases.
The physicians biopsied one of the nodules from the left forearm. Histopathologic evaluation confirmed a benign cavernous vascular lesion, compatible with blue rubber bleb nevus.
Although gastrointestinal screening is not recommended in the affected patients, iron deficiency anaemia may warrant GIT screening. Therefore, this patient was referred to general surgery department for consultation regarding gastrointestinal screening.
Additionally, physicians also considered treatment with sirolimus for this patient. Studies have shown that sirolimus rapidly reduces the size of gastrointestinal lesions and aids in stopping massive gastrointestinal bleeding.
Blue rubber bleb nevus syndrome
Blue rubber bleb nevus syndrome is characterized by multiple venous malformations on the skin and visceral (internal) organs. These lesions which are generally small (1–2 cm), and blue to purple in colour, may present at birth or during early childhood. BRBNS can be autosomal dominantly or it may occur sporadically.
Affected patients may manifest symptoms such as fatigue, hematemesis, melena, or rectal bleeding. Upper- and lower gastrointestinal bleeding is attributable to the spontaneous rupture of the GI lesions. Although, a majority of the patients suffer from chronic bleeding, acute haemorrhage may even lead to death.
In conclusion, those patients who suffer from minor or intermittent gastrointestinal bleeding, should receive blood transfusions and iron supplementation.
For severe haemorrhage, surgical resection, endoscopic sclerosis, laser photocoagulation and treatment with interferon are the treatment options. Corticosteroids, propranalol and sirolimus are some of the other conservative treatment options.
References:
Brandt LJ. Blue rubber bleb nevus syndrome: Capsule endoscopy in a patient with GI bleeding. Gastrointestinal endoscopy. 2007;
Fishman SJ, Smithers CJ, Folkman J, et al. Blue rubber bleb nevus syndrome: surgical eradication of gastrointestinal bleeding. Ann Surg. 2005;241(3):523-528. doi:10.1097/01.sla.0000154689.85629.93
Julia N. Mayba and Kyle CullinghamCMAJ July 29, 2019, 191 (30) E841; DOI: https://doi.org/10.1503/cmaj.190173



