- A Chinese female with an overactive bladder undergoes sacral SNM.
- Two leads placed, one month apart, which gave significant clinical improvement.
- Fat liquefaction after SNM.
- Drainage performed but liquefaction continued.
- Antibiotics started.
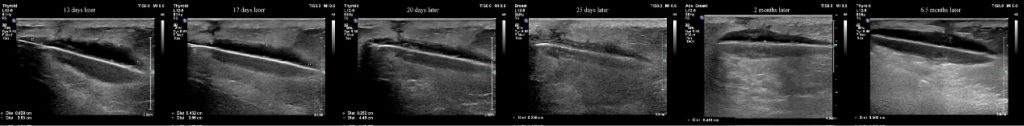
- Significant improvement was seen on serial ultrasounds.
A 26-year-old Chinese female presented to the outpatient department with complaints of urinary frequency, urgency, and incontinence for the past 2 years. The patient’s description of incontinence was consistent with urge incontinence. The patient denied burning micturition or dysuria. She reported voiding at least 20 times during the day and at least 5 times during the night. She also complained of enuresis but had no voiding difficulty.
On examination, the patient was sitting comfortably, conscious, and oriented; the patient’s BMI was 36.33.
Her urine sample was collected for urinalysis, which was negative. The Post-void volume was calculated to be 5 ml.
The patient was diagnosed with an overactive bladder.
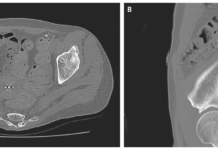
Behavioral therapy showed no benefit; neither did the anti-muscarinic agents. Therefore, she was then suggested to opt for Sacral Neuromodulation. Sacral neuromodulation, also called sacral nerve stimulation, is a medical electrical stimulation therapy. A subcutaneous implantable stimulator is programmed to deliver low amplitude electrical impulses to the sacral nerve.
Stage I and stage II lead placements were performed with an interval of 1 month, as the patient had shown substantial symptomatic improvement (more than 50%) after the first lead placement.
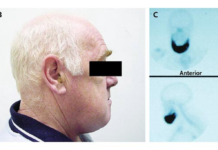
After the stage, II lead placement, the wound tissue liquified and broke on the 7th postoperative day.

Two days later, 6 mL of liquid was aspirated from the wound using the Chinese traditional cupping technique. No further aspirations were required, and the wound was improving. The wound was monitored regularly with ultrasound. Superficial ultrasound showed no obvious liquefaction at the surgical site on the second day.

Six days after the aspiration, a small amount of liquefaction was noticed at the site of the stimulator on ultrasound, which further enlarged ten days later.
The superficial ultrasound revealed mild lead-placement site swelling, but there was reduced liquefaction around the stimulator 17 days later. Apparently, the liquefaction had tracked down to the S3 foramen along the wire.
On serial ultrasounds, progressive reduction of the liquefaction was appreciated at the stimulator site but increased liquefaction and swelling around the puncture.
Oral antibiotics were initiated, which resolved the fat liquefaction within 3 days of the start of medications. Also, the ultrasound showed a progressive reduction in the liquefaction both at the stimulator position and around the lead entry site.
The patient was advised to follow-up regularly, so ultrasounds can be performed to track the changes in fat liquefaction.
Within 2 weeks of discharge, the follow-up ultrasound showed a reduction in the depth of the liquid dark area from 0.628 cm to 0.258 cm.
Reference:
Yang L, Fang W, Wu Y, Li J (2020) Chinese Traditional Cupping Therapy to Treat Fat Liquefaction at SNM Surgery – Case Report. Int Arch Urol Complic 6:072. doi.org/10.23937/2469-5742/1510072