Obstructive pneumonia secondary to foreign body aspiration
This article describes the case of a 68-year-old man with a history of type 2 diabetes mellitus, diagnosed with obstructive pneumonia. According to the patient’s medical history, he underwent tracheostomy in 1993 and right chest rib chondrosarcoma surgery in 1997. He presented to the clinic with complaints of fever and right sided hypochondrium pain. Auscultation of the lungs showed a decrease in breath sounds over the right posterior side of the lower chest.
Doctors referred the patient for a blood test that showed an elevation of inflammatory markers. A chest x-ray was also performed which showed right inferior lung lobe consolidation, consistent with the diagnosis of community acquired pneumonia. He was then admitted with the suspicion.
The patient was referred for a CT scan of the chest which helped with giving the patient a diagnosis
The patient was further advised a CT scan of the chest which showed a foreign body that was not evident on the chest x-ray. The foreign body was located in the inferior right stem bronchus. However, the patient did not have any history or symptoms of foreign body aspiration, for example, recurrent pneumonia, wheeze, dyspnoea, haemoptysis or cough. For further examination, a biopsy was done which showed the presence of granulation tissue. Doctors diagnosed the patient with obstructive pneumonia because of foreign body aspiration. Treatment included piperacilin/tazobactam and short course of corticosteroids. After treatment the patient showed significant improvement.
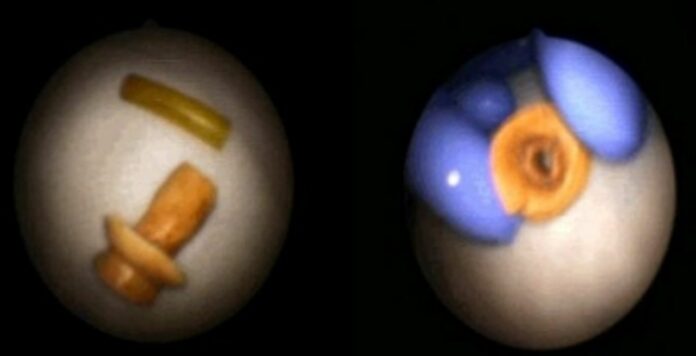
The foreign body was extracted via flexible bronchoscopy, identified as a voice prosthesis. The patient later admitted that he had lost it a while ago. Although foreign body aspiration is more common in children, it can occur at any age. Moreover, the diagnosis is often delayed in adults because of this reason. Similarly, diagnosing obstructive pneumonia is a challenge because of the nature of the foreign body. The clinical and radiological findings are often non-specific and there is no history of choking, as with this case.
Source: BMJ