Cognitive impairment in a patient with a history of homelessness, heavy alcohol use, and malnourishment
Paramedics brought a 48-year-old man who had no fixed place of residence with complaints of confusion and agitation. Initially, the patient could not give history, however, after initial management, he reported self-neglect, heavy alcohol use, and poor diet. On initial examination, he appeared to be thin with an extremely poor general condition. Gross abnormalities were visible in his eyes and skin. His body mass index (BMI) was 14.2, his blood pressure was 75/50, and his body temperature was 33.8°C (hypothermic).
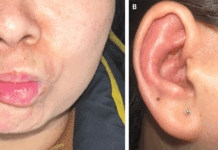
Detailed examination of the skin revealed diffuse follicular hyperkeratosis predominantly on the lower abdomen and the anterior thighs bilaterally. Moreover, lesions on the thighs exhibited crusting and boggy inflammation. Additionally, his face, forehead, and neck harboured inflammatory lesions resembling papular rosacea.

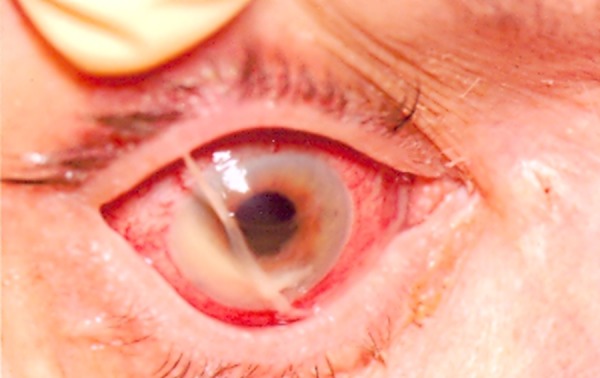
Ophthalmic examination revealed redness in the right eye with sticky discharge. Moreover, the examination of the right eye also revealed a corneal ulcer and a hypopyon. The left eye showed corneal stromal scarring and vascularisation at the site of a healed ulcer.
Past medical history revealed a documented evidence of the previous diagnosis of pulmonary tuberculosis, a healed left corneal ulcer and a surgically treated intertrochanteric fracture of the left hip.
Serology showed mild hypokalaemia, thrombocytopenia, and mildly elevated inflammatory markers. The rest of the results including renal function test, liver function test, calcium, and magnesium were normal. However, blood results revealed deficiency of fat-soluble vitamins, i.e., vitamins A, D, (25-hydroxycholecalciferol) and E. moreover, results revealed an acquired abetalipoproteinaemia due to poor nutrition.
Corneal scrapes from the right eyes grew Streptococcus pneumoniae.
The physicians started the patient on intravenous fluids, intravenous Pabrinex, high-dose parenteral vitamins, urinary catheterization, and topical chloramphenicol in both eyes. Initially, due to the patient’s altered mental status, he was unable to eat orally, however, within a few days, he was having regular meals.
Initially with the management, his electrolytes deteriorated suggesting refeeding syndrome. After 7 days of intravenous replacement, his serology normalised.
For skin lesions the patient received vitamin supplementation, emollients, and the physician counselled him regarding the importance of good personal hygiene.
For his eyes, he received intensive topical treatment with topical ofloxacin and topical atropine. Additionally, he was also prescribed oral doxycycline with gradual addition of topical steroids later on.
Moreover, the dietician recommended a nutritional support menu and oral vitamin supplements.
During the first week of treatment he remained drowsy. By the 12th day he was alert and well-oriented. However, he exhibited cognitive impairment and significant retrograde amnesia. He was unable to retain new information and showed significant cognitive slowing. He scored 18/30 on mini–mental state examination (MMSE) on day 21. Head CT scan revealed significant cerebral atrophy with unusually prominent cerebral sulci, particularly in the frontal and temporal lobes.
His treating physicians believed that his cognitive impairment was multifactorial. Chronic heavy use of alcohol and the associated vitamin B deficiency was one of the causes of his cognitive impairment. However, he did not exhibit features of Korsokoff’s psychosis. Moreover, the patient was also malnourished, therefore, his symptoms may also be attributable to the deficiencies of the fat-soluble vitamins A and E.
Reference:
Dickson JM, Naylor G, Colver G, Powers HJ, Masters P. Multiple vitamin deficiencies in a patient with a history of chronic alcohol excess and self-neglect in the UK. BMJ Case Rep. 2014;2014:bcr2014204523. Published 2014 Sep 22. doi:10.1136/bcr-2014-204523