A 51-year-old non-smoker presents with shortness of breath and gets a diagnosis of a rare disease!
A 51-year-old male presented with complaints of severe shortness of breath for the past 3 years. The patient had no history of smoking.
The patient reported an increase in the severity of his symptoms during the past 1 year. Past history did not reveal any remarkable findings, i.e., he had no history of fever, weight loss, or hemoptysis. Neither history revealed any chronic infection, including tuberculosis.
On chest auscultation, the physician appreciated bibasilar crackles. The readings on the pulmonary function test indicated subtle restrictive findings. Blood reports revealed no pathologic findings.
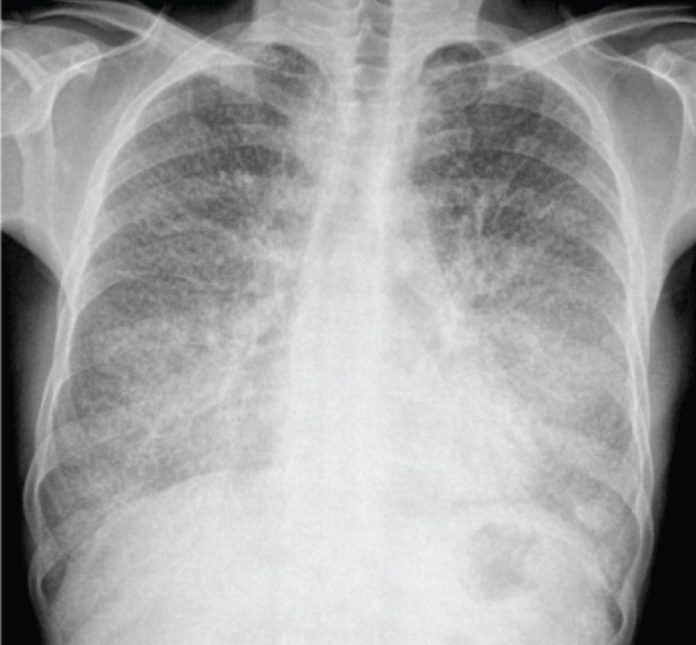
A plain radiograph of the chest showed, dense, numerous, diffuse micronodular opacities bilaterally but predominantly in the lower zones.
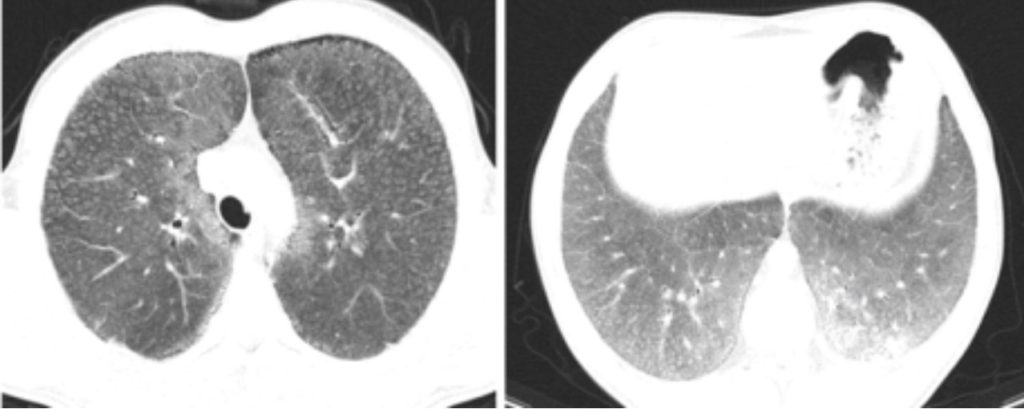
Computed Tomography (CT) scan of the chest concurred with CXR findings by revealing symmetrical lower lobe predominant diffuse, nodular, intra-alveolar opacities of calcific density. Additionally, CT scan showed diffuse septal thickening secondary to calcification was appreciate along with diffuse ground-glass attenuation (crazy-paving pattern) and subpleural multiple small cysts (black pleura sign).
His doctors performed a transbronchial biopsy which confirmed the diagnosis of Pulmonary Alveolar Microlithiasis (PAM).
Pulmonary Alveolar Microlithiasis
Pulmonary Alveolar Microlithiasis (PAM) is a rare chronic lung disease which is characterized by bilateral diffuse innumerable minute intra-alveolar deposition of spherical calcium and phosphate bodies (microliths). The exact aetiology is unknown, however, researches show that it is secondary to the mutation in the sodium cotransporter (SLC34A2) gene.
Patients with PAM usually present anytime between birth and 40 years. However, one-fifth of the case may present after 40 years of age. PAM has a slight predominance for males. Most of the patients present incidentally on imaging, as the majority may have no symptoms. However, those who have symptoms. They may present with restrictive symptoms such as dyspnea (shortness of breath), non-productive cough, and chest pain.
CXR and chest CT scan show pathognomonic findings. Those characteristic findings include numerous, diffuse, bilateral, sand-like, calcific micronodular infiltration, thin-walled subpleural cysts, ground-glass attenuation, diffuse calcifications, subpleural and parenchymal nodules, interlobular septal calcifications and subpleural cysts.
Although there are pathognomonic imaging findings, histopathological evaluation of a biopsy sample must be done to confirm the diagnosis.
The only effective therapy for PAM is lung transplantation. Steroids and repeated therapeutic bronchoalveolar lavage have no role in management. However, some studies support the use of disodium etidronate therapy. Nonetheless, affected patients should be closely followed for signs of respiratory failure as the average time to develop respiratory failure is usually 10–15 years after diagnosis.
Reference:
Cengiz A, Büyükterzi M, Aybay MN, Sivri M, Cengiz A, et al. (2017) An Unusual Cause of Shortness of Breath in an Adult Man: Alveolar Microlithiasis. Clin Med Img Lib 3:068. doi.org/10.23937/2474-3682/1510068