Development of methotrexate-associated lymphoproliferative disorder ectopically in the maxillary gingiva and bilateral lungs.
A 58-year-old Japanese woman presented to the Department of Dentistry and Oral Surgery, Tsuyama Central Hospital (Okayama, Japan) in May 2018 with a painful right maxillary premolar and an ulcer with a 2-weeks history. The patient given a diagnosis of rheumatoid arthritis 10 years ago. Moreover, was under treatment with immunosuppressive drugs, including methotrexate and prednisolone. She was diagnosed with methotrexate-associated lymphoproliferative disorder (MTX-LPD).
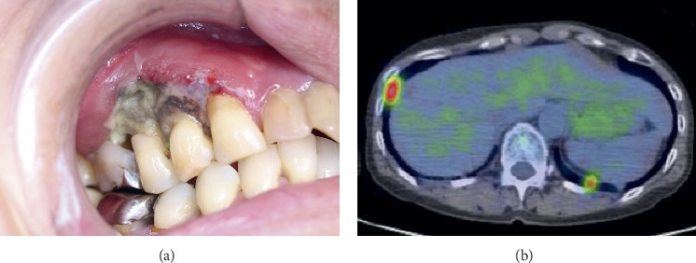
Clinical examination showed a swollen submandibular lymph node with pain. Similarly, intraoral examination was consistent with swelling and a necrotic ulcer in the right maxillary gingiva, in the region of the canine and the first molar. Although, there was no exposure of the alveolar bone. The premolar, however, showed mild mobility with pain on biting and percussion. The patient’s blood test was positive for an EBV infection.
Examination and diagnosis
Dental radiographs and CT scan of the head and neck did not show any signs of bone destruction with the lesion. There were no lymph node swellings except for the right mandibular lymph node. Although chest CT revealed a nodular mass, suspecting it to be a malignant tumour of the bilateral lungs. Additionally, fluorodeoxyglucose-positron emission tomography/CT (FDG-PET/CT) showed the presence of an increased uptake in the bilateral lungs and right maxilla. However, there was no uptake in the right submandibular lymph node.
Doctors were suspecting methotrexate-associated lymphoproliferative disorder. The patient was under treatment with MTX for almost a year. Therefore, the lesion was biopsied based on this suspicion. In addition, a large-sized lymphocyte infiltration was noted with hematoxylin and eosin staining with a background of inflammatory cell infiltration in the submucosal stroma.
Immunohistochemistry showed an atypical large-sized lymphocytes. EBV-encoded small RNA in situ hybridization was positive. In addition, histopathology was consistent with EBV-positive diffuse large B-cell lymphoma (DLBCL). The patient did not consent to an endoscopic biopsy, so, it was not possible to diagnose the bilateral lung lesions. However, the lung lesions were also MTX-LPD as confirmed by a hematologist and respiratory medicine physician at another hospital.
The patient was diagnosed with MTX-LPD. The disorder developed ectopically and expressed in the maxillary gingiva and bilateral lungs.
Treatment
After consulting the patient’s primary physician, the doctors decided on discontinuing MTX treatment. The ulcer and gingival lesion reduced significantly. The swelling and pain in the right submandibular lymph node resolved completely. The size of the bilateral lungs nodular mass also began to reduce. At 4 weeks of discontinuing MTX, the ulcer disappeared completely. Although, shedding of necrotic gingiva caused exposure of the perilesional bone. In addition, the exposed bone necrosed at 5 weeks. Similarly, the sequestrum along the premolar was removed under local anaesthesia.
The wound was covered with epithelium two weeks after surgery. The lesion completely resolved. At 15 months of withdrawal from MTX the patient showed no recurrence and was in good condition.
References
Methotrexate-Associated Lymphoproliferative Disorder Developed Ectopically in the Maxillary Gingiva and Bilateral Lungs https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7204348/



