A case of a rare cause of anaemia and myeloneuropathy- copper deficiency!
Here is a case presentation of a female patient with myeloneuropathy secondary to copper deficiency. A 54-year-old female patient was referred after a suicide attempt with a suspected diagnosis of neuropathic pain. The patient complained of progressive painful paraesthesia in her feet spreading to her thighs. She had similar complaints in her hands too. Moreover, the patient also complained of leg weakness and imbalance for the past 6 months, due to which she has become dependent.
Her surgical history revealed that she had undergone multiple bariatric surgeries starting with jejunoileal bypass at 15 years of age. Thereafter, the patient required multiple revisions and a Roux-en-Y gastrojejunostomy at age 47 years.
Nutritional history revealed a standard diet. Also, she took supplemental vitamins A, D, E, K, B12 and iron.
On examination, she had quadriparesis, diffuse hyperreflexia excluding the masseter and Achilles reflexes. Additionally, she had severe proprioceptive and vibration sense loss.
Therefore, the patient’s surgical history and examination findings suggested myeloneuropathy secondary to malabsorption syndrome.
Serological tests showed normocytic anaemia, normal vitamin B12 and zinc levels. however, she had low copper level of 3.9 (normal 10–22) μmol/L.
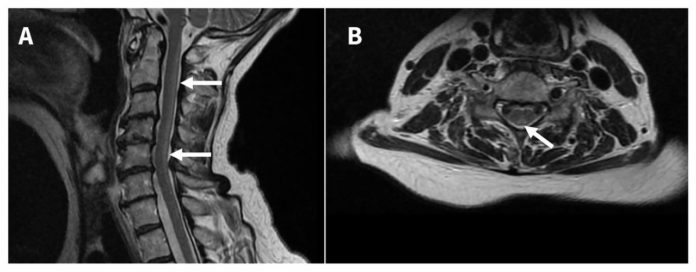
Her doctors performed magnetic resonance imaging (MRI) of the cervical spine, which showed longitudinally extensive inverted “V” T2 hyperintensity of the posterior column. The MRI findings suggested a diagnosis of B12 or copper deficiency.
Since the patient had low levels of copper, she received a diagnosis of copper deficiency myeloneuropathy (CDM).
The patient received oral and intravenous copper supplementation. She showed functional improvement in the first few months. Eventually, she improved enough allowing her to transfer with assistance and operate a wheelchair.
Copper deficiency:
Acquired copper deficiency is one of the rare causes of anaemia, albeit a treatable one. It causes non-compressive myelopathy which resembles the subacute combined degeneration due to vitamin B12 deficiency.
Patients with CDM most commonly present in the 5th and 6th decades with a female predilection (F:M = 3.6:1).
About 20% of the patients have no identifiable cause. However, some of the risk factors of CDM include:
- Previous upper gastrointestinal surgery
- Excess zinc
- Malabsorption syndromes
Approximately, 10-20% of the patients who have undergone Roux-en-Y gastrojejunostomy develop copper deficiency, therefore, it is recommended to give postoperative copper supplementation.
Patients with copper deficiency should be treated with intravenous or oral copper. Thereafter, serum copper levels can be checked to see the response.
References:
Jaiser SR, Winston GP. Copper deficiency myelopathy. J Neurol. 2010;257(6):869-881. doi:10.1007/s00415-010-5511-x
Alexander J. Arnold, Aleksander Tkach and Daryl J. Wile, CMAJ August 06, 2019 191 (31) E866; DOI: https://doi.org/10.1503/cmaj.190168



