Gradenigo’s syndrome (GS) is a triad of unilateral periorbital pain, diplopia, and persistent otorrhea. A 57-year-old male presented with clinical manifestations of GS for the past 1 month. He presented with diplopia on the left lateral gaze and headache on the left side (hemicranial pain). The patient also complained of decreased sensation on the left side of his face.
History:
The patient had a history of left ear infection 1 year back. Antibiotics resolved his ear infection back then.
Examination:
Examination of the ears revealed normal tympanic membranes bilaterally. Mastoid tenderness was absent. Tuning fork tests gave the following results:
- Positive Rinnes tests bilaterally.
- Weber was centralized.
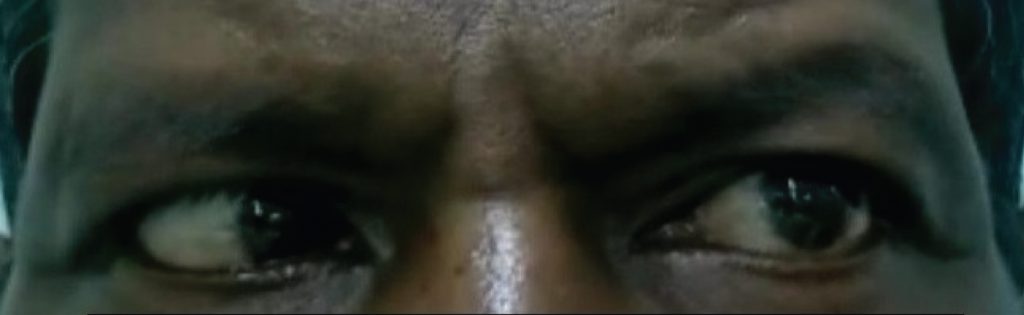
Examination of the eyes revealed the restricted lateral movement of the left eye. Hence pointing to left abducens nerve palsy. The vision was good in both eyes with normal fundoscopy bilaterally.
There were no other positive findings on the ENT and cranial nerve examinations.
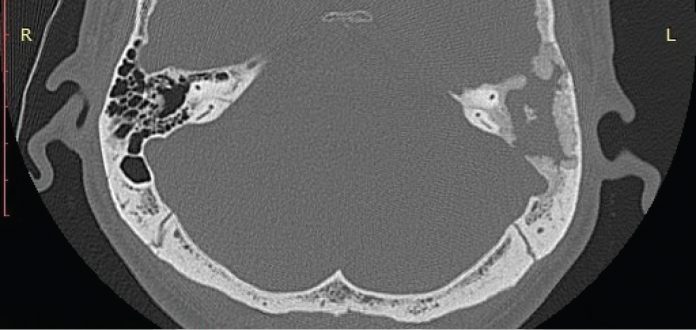
High-resolution computed tomography (HRCT) of the temporal bone showed complete erosion of left mastoid aircells. The findings suggested left otomastoiditis, along with the erosion of the dural and sinus plate with extradural intracranial extension (Figure 2).
MRI Brain and orbit were normal, and so was MR Venogram.
Pure tone audiometry (PTA) results suggested mild conductive hearing loss on the left side while right was normal.
The patient was diagnosed with Gradenigo’s syndrome.
Gradenigo’s syndrome (GS):
GS, which involves the trigeminal nerve (fifth cranial nerve) and Abducens nerve (the sixth cranial nerve) presents with symptoms of unilateral periorbital pain, diplopia, and persistent otorrhea. It is associated with bacterial otitis media with petrositis.
Although, antibiotics have minimized the incidence of Gradenigo’s syndrome, still some cases may surface; hence knowledge regarding the disease is essential.
The doctors planned a left mastoidectomy for the patient, so they performed relevant serological investigations. They started him empirically on oral ciprofloxacin
Ciprofloxacin partially helped the left abducens palsy.
The patient underwent left cortical mastoidectomy. The surgery revealed pale, dense, avascular granulations in the mastoid and middle ear cleft. External auditory canal’s (EAC) posterior-superior wall was partially destroyed with an intact tympanic membrane.
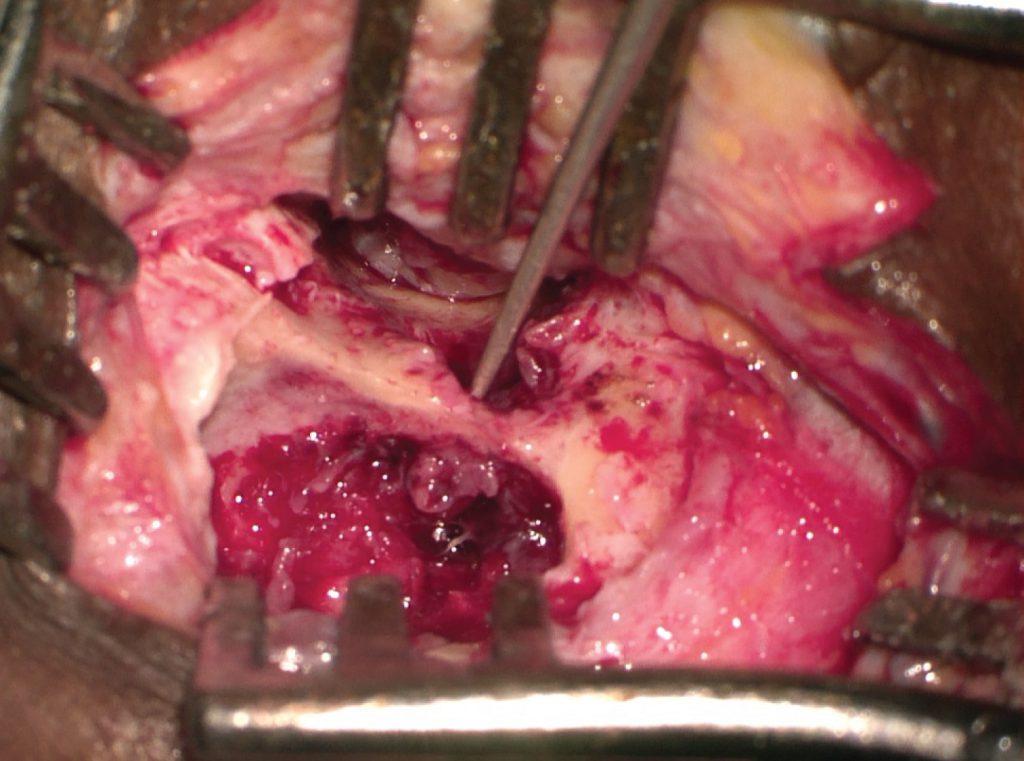
The surgeons cleared of the granulations and sent the collected sample for histopathology and Genexpert. They closed the defect in the external auditory canal wall with a cartilage.
Histopathology revealed chronic inflammatory granulations. Genexpert was negative for tuberculosis.
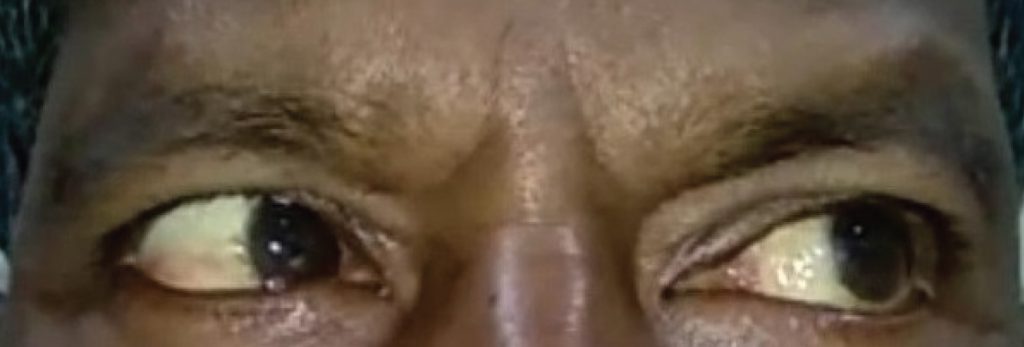
Since the patient was responding, he received ciprofloxacin for 3 weeks. The lateral rectus palsy completely resolved.
Possible complications of Gradenigo’s syndrome:
It is imperative to be aware of this rare disease to make an accurate diagnosis. Prompt investigations and treatment are crucial to decrease the fatality of the disease. Some of the complications of GS include intracranial abscess, meningitis, Vernet’s syndrome, prevertebral abscess, and parapharyngeal abscess
References:
Pedroso JL, de Aquino CC, Abrahão A, et al. Gradenigo’s Syndrome: Beyond the Classical Triad of Diplopia, Facial Pain and Otorrhea. Case Rep Neurol. 2011;3(1):45-47. Published 2011 Feb 15. doi:10.1159/000324179
Allam AF, Schuknecht HF (1968) Pathology of petrositis. Laryngoscope 78:1813–1832
Motamed M, Kalan AGradenigo’s syndromePostgraduate Medical Journal 2000;76:559-560.
Sathe NU, Kaku DR, Taku A, Pawara M, Gupta VK (2020) A Rare Presentation of Gradenigo’s Syndrome. J Otolaryngol Rhinol 6:091. doi.org/10.23937/2572-4193.1510091



