An 84-year-old man with a history of aortic stenosis for which transcatheter aortic valve replacement (TAVR) was performed seven days back, complains of severe pain and weakness in his right arm. The pain was sudden in onset.
Examination of his right hand revealed reduced strength, nonpalpable peripheral pulses (radial and brachial pulses), and pale forearm.
Three-dimensional computed
tomographic angiography was performed, which revealed right axillary arterial
occlusion (Panel A, arrow).
The two-dimensional angiogram showed hypoattenuated thickening of the
noncoronary and left coronary aortic leaflets (Panel B, arrows).
Thrombus was removed by surgical thrombectomy, and the patient was prescribed aspirin and clopidogrel. Post-operative transesophageal echocardiography was performed, which showed no thrombus in the heart; however, a thickened noncoronary aortic leaflet was spotted. The transvalvular gradient was measured at 15 mm Hg, an increase from 8 mm Hg measured after TAVR.
The patient’s symptoms of pain and weakness alleviated after the surgical thrombectomy. Aspirin and clopidogrel were discontinued, and oral anticoagulant was initiated.
Transcatheter aortic valve replacement (TAVR), also called transcatheter aortic valve implantation, is a surgery to replace severely disease aortic valve. The beauty of this procedure is that it is minimally invasive. Owing to this characteristic, TAVR has greatly replaced surgical aortic valve repair.
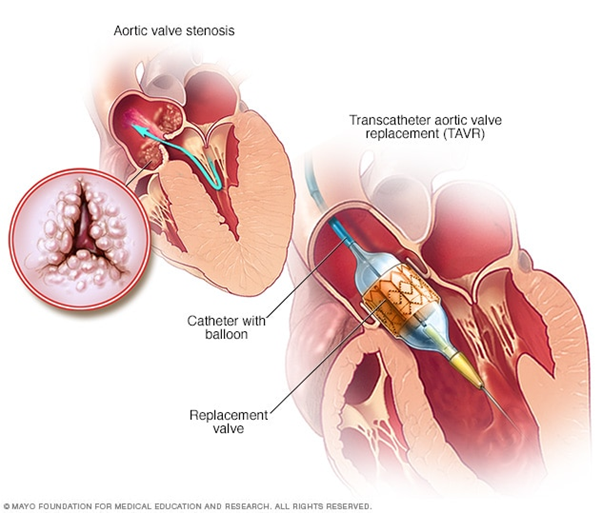
Image Source: Mayoclinic©
However, TAVR has its own set of side effects.
The risks associated with TAVR include:
- Bleeding
- Thromboembolism
- Infection
- Contrast-induced kidney damage
- Valve slippage
- Valve leakage
- Arrhythmias
- Death
Despite the efforts at eliminating the adversities associated with TAVR, the risks of thrombosis, and cerebral ischemia after the TAVR are still significant enough to require special attention. Therefore anticoagulants and antithrombotics are given post-TAVR to reduce the risk of thrombotic events. However, these medications increase the risk of bleeding, which also has its consequences.
What increases the thrombotic potential after TAVR?
There is no single factor to be named here. The mechanism is multifactorial. The disturbance in the flow of blood due to the newly replaced prosthetic valve plays a major role. Other contributing factors can be the prothrombotic metallic frame and a patient with comorbidities which increase the thrombotic tendency.
Thrombi usually form on the aortic side of the implanted valve. This fibrin rich thrombus may dislodge and occlude any other vessel in the body, for instance, the axillary artery in the case in discussion here.
There are limited studies to determine the best approach to prevent thrombosis after TAVR without increasing the risk of bleeding. Novel anticoagulants and antithrombotics are used on an individual basis. However, there is a dire need for developing safer and potent TAVR-specific antithrombotics.
References
Alexander Kille, M. a. (2020, January 09). Axillary Artery Occlusion after TAVR. Retrieved from The New England Journal of Medicine: https://www.nejm.org/doi/full/10.1056/NEJMicm1913768
Ranasinghe, M. P., Peter, K., & McFadyen, J. D. (2019). Thromboembolic and Bleeding Complications in Transcatheter Aortic Valve Implantation: Insights on Mechanisms, Prophylaxis, and Therapy. Journal of clinical medicine, 8(2), 280. https://doi.org/10.3390/jcm8020280




