Case Report
Interstitial pregnancy also defined as an ectopic pregnancy implanted in the proximal or interstitial tubal segment, which crosses the myometrium. For example trophoblastic tissue implantation in the tubal stump following salpingectomy. Interstitial pregnancies make up 2–4% of all tubal pregnancies. The incidence of ectopic pregnancies is typically increasing. But there appears to be a parallel increase in the number of interstitial pregnancies. This increase is most likely related to better diagnosis, ipsilateral salpingectomy, existing damage from previous ectopic pregnancy, use of assisted reproductive technologies (ART). And increased prevalence of pelvic inflammatory disease, some of which are known risk factors for ectopic pregnancy in general.
Interstitial pregnancy has an estimated maternal mortality incidence of up to 2.5%. That is seven times higher than that of ectopic pregnancies. The higher morbimortality is owing to the possibility of catastrophic bleeding. On the one hand, the cornual area has essential vascular anastomoses connecting uterine and ovarian veins, specifically the arcuate vessels. However, when compared to the other segments of the tube, the interstitial section has a substantially greater potential to expand before rupture. It includes the absence of symptoms until later, reaching a rate of uterine rupture of 20% in pregnancies that develop beyond 12 weeks.
High-resolution transvaginal ultrasound and sensitive quantitative beta-human chorionic gonadotropin (β-hCG) testing have made it possible to diagnosis interstitial pregnancies as early as 6.9-8.2 weeks, especially with a high clinical suspicion. Early diagnosis is critical for successful treatment and positive outcomes in individuals with this kind of ectopic pregnancy.
This is a rare case of spontaneous twin interstitial pregnancy with embryonic cardiac activity.
Case Presentation
A healthy Portuguese white woman in her early forties (gravida 2, para 0) came to our hospital for an early pregnancy examination. After having an uneventful right laparoscopic salpingectomy for tubal isthmic ectopic pregnancy three months prior. Despite being asymptomatic, she experienced 6 weeks and 4 days of amenorrhea and tested positive for β-hCG in her urine.
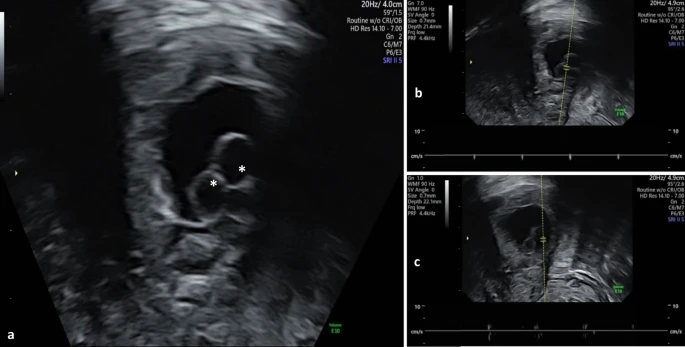
She was hemodynamically stable, and the physical examination was unremarkable. Transvaginal ultrasound revealed an empty uterine cavity. And an eccentric gestational sac on the right side of the uterine fundus, contained within the uterine serosa. But a thin band of myometrium separated the uterine serosa from endometrial cavity. The gestational sac measurements were consistent with the last menstrual cycle. It consisted of two yolk sacs and two embryonic poles with cardiac activity with no amniotic membrane. These ultrasonographic findings suggested a twin right interstitial pregnancy.
Management
After discussion of ultrasound results with the patient. Management options along with their implications, and prognosis were reviewed. That includes expectant management, systemic methotrexate (MTX) therapy, and surgical intervention. Given the presence of viable embryos, expectant management was ruled out. Surgical therapy was the definitive choice due to existence of fetal cardiac activity, along with the patient’s choice of fertility-sparing approach.
One day following hospital admission, the patient underwent a four-port laparoscopy with optic trocar entrance while under general anesthesia. During the examination, an unruptured bulging mass of around 25 mm discovered at the right uterotubal junction, confirming the diagnosis of interstitial pregnancy. Proximal temporary bilateral uterine artery cutting was performed.
A cornuostomy was also performed. That involved making a full-thickness linear incision along the cornual mass and distal to the suture with a monopolar hook. In this way the trophoblastic was removed without entering the endometrial cavity. Bipolar cauterization helped to stop the bleeding. The uterine artery clamps were removed with an absorbable adhesion barrier placed above the suture. Blood loss during the surgery estimated to be roughly 100 mL.
The patient discharged on the second post-operative day. Adjunctive treatment was unnecessary, and the patient was asymptomatic at the 6-week postoperative visit. Histological investigation confirmed the diagnosis of interstitial pregnancy. One year following the diagnosis, the patient was still attempting a spontaneous pregnancy.
Discussion and Conclusion
Angular pregnancy is not a clinical phenomenon; rather, it refers to a eutopic pregnancy implanted in the upper lateral aspect of the uterine canal, medial to the uterotubal junction. Similarly, the term “cornual” meant both normally sited pregnancies in the lateral aspect of the uterine cavity and ectopic pregnancies, namely interstitial pregnancies or gestations located in the rudimentary horn of a unicornuate uterus, with the latter being the only one that should receive this designation.
In this case, a single gestational sac containing two yolk sacs and two embryonic poles with cardiac activity indicated a monochorionic twin pregnancy. Although the quantity of yolk sacs is occasionally used to predict amnioticity in early gestation, it is not always reliable. Furthermore, the absence of a visible amniotic membrane at this stage does not rule out diamnioticity, as sonographic detection may be delayed. As a result, while monochorionicity has been verified, amnionicity remains undetermined.
Diagnosing interstitial pregnancy requires clinical suspicion, serum β-hCG tests, transvaginal ultrasound, and diagnostic laparoscopy.
Interstitial pregnancy diagnostic criteria via ultrasound include: (1) gestational sac located outside the uterine cavity, (2)partial surrounding of the sac by myometrium, and (3) visualization of the interstitial line sign. That shows an intramural segment of the Fallopian tube next to the gestational sac and uterine cavity.
Medical management is the primary treatment for asymptomatic patients. If unruptured interstitial pregnancy detected early in the first trimester. This management involves administering Methotrexate (MTX) either systemically (intravenous or intramuscular) or locally, under ultrasound guidance. Local administration, though more invasive, has the advantage of fewer systemic side effects but is operator-dependent. It requires specialized facilities and trained personnel, which makes it less accessible and more expensive compared to systemic administration.
Surgical management is the definitive treatment for interstitial pregnancy, indicated in cases of hemodynamic instability, significant symptoms, cornual rupture, large pregnancies, or heterotopic pregnancies.