Case Report
Struma ovarii (SO) is an uncommon ovarian tumor that contains at least 50% thyroid tissue. It accounts for around 1% of all ovarian cancers and 2.7% of dermoid tumors. Malignant transformation occurs in about 0.17-1.4% of cases. Despite its mostly benign nature, the rarity of SO and the possibility of malignancy highlight the need for attention and prompt identification. SO is typically diagnosed with a histopathological study. Laparoscopic surgery is the most effective treatment for benign cases of SO.
The prognosis for benign struma ovarii and malignant cases with no metastases is generally positive. Malignant SO typically has a good prognosis, but with metastasis, the prognosis becomes less favorable. Notably, this paper includes a comprehensive description of diagnostic and treatment techniques for struma ovarii.
Case Presentation
A 68-year-old Chinese female arrived to the endocrine surgery department with a 6-month history of recurrent urethral outlet tumescence and a recently detected left adnexal tumor. Her medical and drug history was ordinary, and there were no significant family medical concerns. She had four pregnancies, four vaginal deliveries, and one infant died; she now has three children.
Investigations
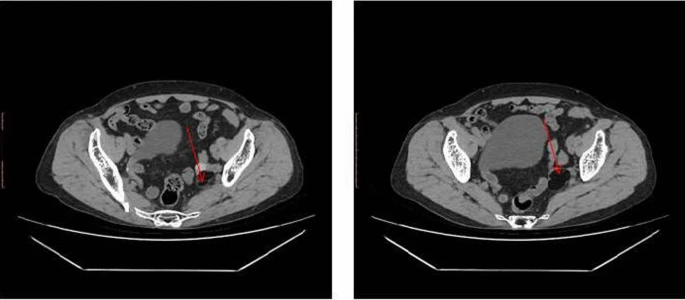
Routine laboratory measures, thyroid function tests, and tumor marker assessments, including cancer antigen (CA)-125 and CA19-9, were all within normal limits and revealed no significant abnormalities. Pelvic CT scans indicated an irregular mass in the left adnexal area, measuring approximately 24 mm × 38 mm × 51 mm. This tumor had various densities, including parts that resembled fat, indicating a teratoma. Following hospitalization and physical examination, a palpable lump was discovered in the same place. A transvaginal ultrasound revealed a solid mass of approximately 28 mm × 19 mm, confirming the preliminary diagnosis of a teratoma. The following day, pelvic magnetic resonance imaging (MRI) revealed an irregular mixed signal mass of similar size, switching between high and low signal intensities, indicating a complicated teratoma.
The patient then underwent a laparoscopic left adnexectomy. Histopathological examination revealed a mature cystic teratoma with thyroid tissue development in the left ovary. At the time of writing, the patient is alive and enjoying an excellent quality of life, with no bulk seen on imaging.
Discussions
Struma ovarii (SO) is an uncommon ovarian teratoma primarily made of thyroid tissue. It typically affects women between the ages of 40 and 50, with a peak incidence reported in those aged 30-40 who have not yet reached menopause. Despite much investigation, the specific cause of SO remains unknown. SO is difficult to diagnose because roughly 40% of patients are asymptomatic and discovered by chance during routine ultrasound. Blood flow signals within or on the tumor’s wall, as well as ascites, might make identification from malignant ovarian tumours even more difficult.
This case study shows ultrasound photos of a benign simple ovarian goiter that appeared as a solid mass during examination. Symptomatic instances may demonstrate pelvic pain, abdominal distention, menstrual abnormalities, and symptoms of hyperthyroidism.
Additionally, thyroid dysfunction might be detected in 5-8% of individuals. Distinguishing SO from other adnexal tumors, such as mature cystic teratoma, mucinous cystadenoma, fallopian tube abscess, and ovarian cancer with thyroid-like differentiation, is critical yet difficult due to shared histological characteristics. A thorough examination of clinical, radiological, and histological data is required for an appropriate diagnosis.
Imaging techniques such as CT scanning and MRI can help determine disease severity and its influence on nearby organs. Surgical surgery remains the cornerstone of SO treatment, with several reported outcomes indicating a favorable prognosis. In our case, due to suspicion of ovarian cancer, laparoscopic left appendage resection was performed, coupled with uterine rectus abdominis muscle suspension and anterior vaginal wall repair, resulting in full excision of the left appendage.