Penetrating neck injuries (PNI) are not so common, representing 5-10% of all trauma patients. The most common mechanism is stabbing followed by a gunshot. Other possibilities include road traffic accidents and high-velocity trauma. Though rare, but the mortality rate is as high as 10%. Penetrating neck trauma is both dangerous and challenging because of all the vital structures lie in that small area, from the neurological meshwork including the spinal cord, cranial nerves, peripheral nerves to aerodigestive systems, let alone the major blood vessels.
Above shown is a picture of a 45-year-old man who was brought to the ER after being stabbed in the neck in an event of street robbery. This happened when the victim resisted the robbery and things went south. The patient ended up in the ER with a knife buried on the back of his neck.
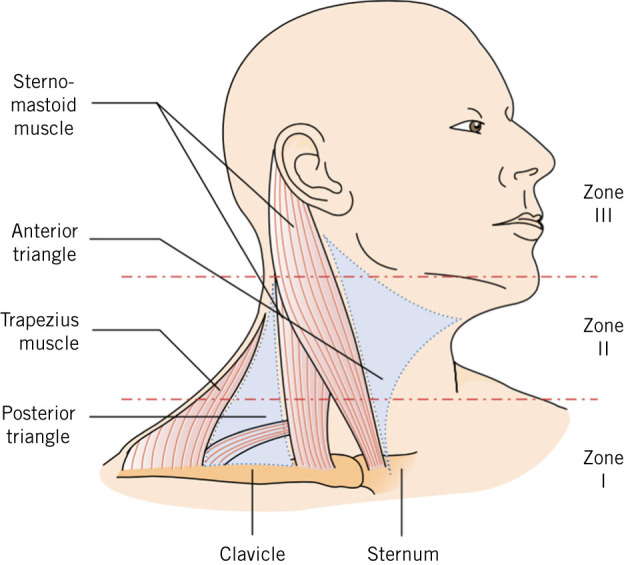
Penetrating neck trauma is divided according to the affected zones. Three zones have been described, zone I being the most caudal one with the highest mortality rates, while zone II is the mid-neck which is the most commonly affected. The upper neck is zone III, from above the angle of the mandible to base of the skull. What seems as zone I externally might be involving zone II internally, so an imaging study is essential in this regard. طريقة لعب القمار
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5849205/
Clinical presentation is the best immediate guide to the affected structures. For example, dysphagia with oesophagal injury, hoarseness with tracheal injury or with injury to recurrent laryngeal nerve, neurological manifestations with spinal cord injury, etc. العاب على الهاتف Airway tract injury can not only lead to respiratory distress but also pneumothorax and subcutaneous emphysema can ensue.
En route to the emergency department, the patient should be regularly assessed for breath sounds and vitals should be frequently recorded. If tension pneumothorax is suspected, needle thoracostomy should be immediately performed. The impacted weapon should not be removed on the scene or en route. The protocols for resuscitative measures and cervical spine immobilization should be exercised.
PNI patients may deteriorate rapidly, therefore demand immediate attention.
Such trauma patients are initially assessed for violation of platysma muscle. If platysma is not intact then it is a penetrating injury and further assessment for evaluation of damaged structures is to be carried out. العاب كازينو مجانية If platysma is intact, then the wound is superficial. The standard of care for unstable patients with PNI is surgery, depending upon the injured zone of the neck. Whereas, for stable patients, a multidetector computed tomography with angiography (MDCT-A) has shown to be beneficial in directing the line of management.
The case in discussion is a miracle. The knife, fortunately, missed the spinal cord by a few millimetres. Surgeons were able to remove the knife without any neurological consequences. Smooth postoperative recovery was reported.
References
Daniel Mark Alterman, R. M., & Chief. (2018, April 10). Penetrating Neck Trauma. Retrieved from Medscape: https://emedicine.medscape.com/article/433306-overview
Nowicki, J. L., Stew, B., & Ooi, E. (2018). Penetrating neck injuries: a guide to evaluation and management. Annals of the Royal College of Surgeons of England, 100(1), 6–11. DOI:10.1308/rcsann.2017.0191




